Most patients still receive total hip arthroplasty

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteonecrosis is a potentially devastating disorder of various joints including the hip, knee, shoulder and ankle and can progress to end-stage arthritis. Osteonecrosis has many causes, with corticosteroids and alcohol abuse accounting for over two-thirds of cases. The pathophysiology and pathology of osteonecrosis is similar regardless of etiology, with bone death leading to joint collapse and eventual arthritis. The treatment of this disease aims to halt the progression or delay the onset of arthritis.
The treatment of osteonecrosis of the hip (also known as avascular necrosis or AVN) has evolved over the past two decades. Multiple treatment options are available for this younger population of patients based on their disease stage and progression, orthopaedist’s experience and patient preference. However, once substantial joint surface collapse has occurred, or signs of degenerative arthritis appear, total joint arthroplasty becomes the most appropriate treatment option. Osteonecrosis cases make up an estimated 10 percent of all total hip arthroplasties performed annually in the United States. However, the utilization of treatment options for hip AVN is currently unknown.
Therefore, we conducted an analysis of the National Surgical Quality Improvement Program (NSQIP) surgical outcome database to determine the trends of surgical treatment of hip osteonecrosis between 2008 and 2014. Using ICD-9, we identified 3,958 cases of hip osteonecrosis that underwent surgical treatment during this time period. We determined annual distribution of surgical treatments for all specific procedures and for joint-sparing versus joint-replacing procedures. The overall number of surgical procedures performed annually increased from 88 to 1,161 between 2008 and 2014. The rate of total hip arthroplasty performed has increased during this time period from 81 percent in 2008 to 95 percent in 2014. Although the number of joint-preserving procedures increased during this time period, the percentage of preserving procedures decreased annually.
Advertisement

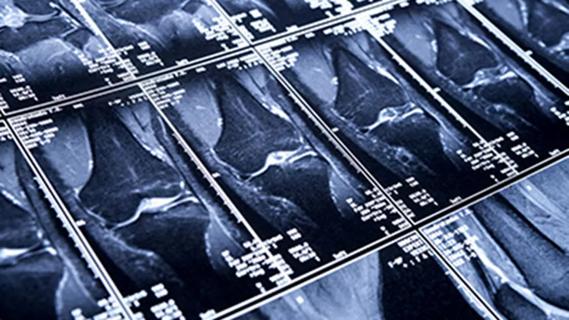
MRI of hip osteonecrosis. Arrow indicates a necrotic zone
The findings of this study validate previous reports that found total hip arthroplasty to be the most common procedure performed for treatment of osteonecrosis of the hip. The results also demonstrate an increasing number of procedures performed for osteonecrosis, suggesting higher awareness of this disease.
Operative interventions for early stage disease include joint-preserving procedures such as core decompression, with or without the use of bone grafts, and biologic agents such as bone morphogenetic proteins (BMP), or cell-based therapy. These procedures first evacuate the necrotic bone through a window in the femoral head-neck junction and subsequently fill the defect with a combination of the above-mentioned materials. At Cleveland Clinic, some of these treatments, such as BMPs, percutaneous drilling and the “trapdoor” procedure, which replaces the dead bone with cancellous and cortical autograft, are being studied and have been quite successful. These joint-preserving procedures are usually attempted in precollapse lesions, when the articular cartilage is generally intact with only the underlying subchondral bone affected.
Conversely, after severe subchondral collapse has occurred, procedures that attempt to salvage the joint are rarely successful, and joint arthroplasty is necessary to relieve pain. Joint arthroplasties, such as hip resurfacing and total hip arthroplasty, are chosen depending on the extent of the disease. Fortunately, reports have shown successful results for these procedures utilizing modern prostheses.
Advertisement
Dr. Mont is Chair of the Department of Orthopaedic Surgery.
Advertisement
Advertisement

Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients

How to diagnose and treat crystalline arthropathy after knee replacement

Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network

Reduced narcotic use is the latest on the list of robotic surgery advantages

Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals

Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions