A customized approach to diagnosis and corrective repairs is key
By Nicholas Smedira, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Classically, left ventricular outflow tract obstruction (LVOTO) was identified when symptomatic patients were found on echocardiography to have a septum measuring approximately 20 mm and had LVOTO at rest or when provoked by a Valsalva maneuver or administration of amyl nitrate.
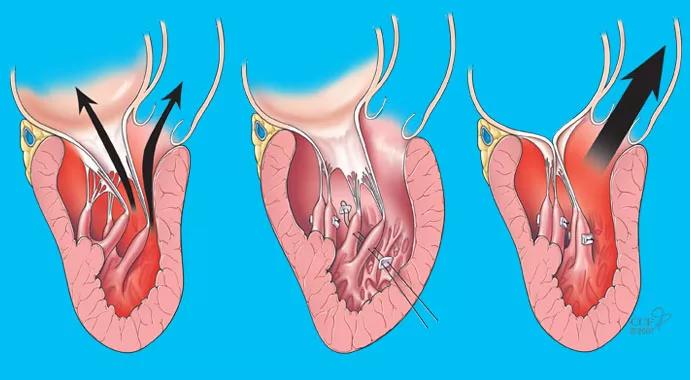
When LVOTO due to this severity of septal hypertrophy is identified, treatment is straightforward: A myectomy or an alcohol septal ablation is performed, which eliminates the obstruction. The patient’s symptoms improve or completely disappear.
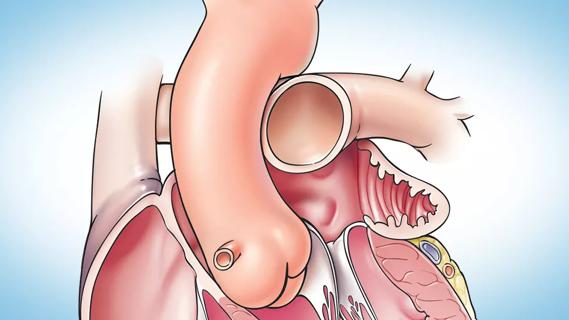
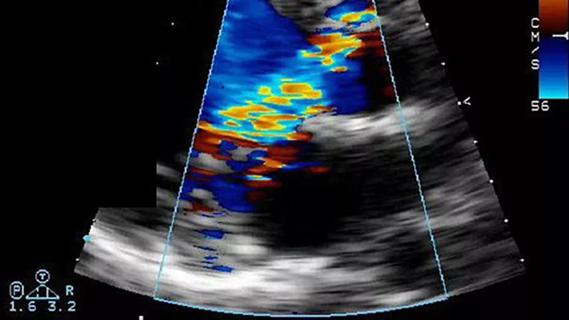
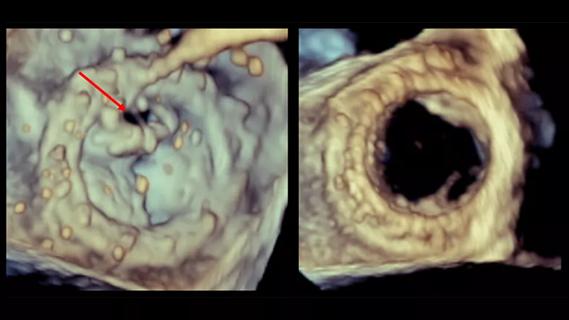
At Cleveland Clinic we are identifying increasing numbers of patients who have LVOTO with minimal to mild left ventricular (LV) hypertrophy (septum of 13 to 17 mm) (Figure). It is not known which of the following these cases of mild or no hypertrophy represent:
While these cases can be much more difficult to diagnose, our imaging experience has grown and our surgical arsenal has expanded, yielding more tools than ever to diagnose and treat these clinically challenging symptomatic patients who present with relatively normal resting echocardiographic images.
Patients in this subgroup with LVOTO and mild or no hypertrophy often present a diagnostic dilemma. The lack of hypertrophy and absence of a resting gradient mean a more aggressive diagnostic approach (such as with amyl nitrate or exercise stress testing) is needed. Moreover, if such tests are performed and the LVOTO is identified, options are limited because there is insufficient hypertrophy for alcohol ablation or substantial myectomy to open the outflow tract.
Advertisement
These constraints have prompted us to develop new diagnostic approaches and surgical techniques to identify and treat LVOTO with minimal hypertrophy. In such cases, often seen in young and healthy patients, we typically perform a stress echocardiogram during vigorous exercise on an upright bicycle. This avoids the rapid heart rate recovery seen with standard treadmill testing and increases the chance we will provoke obstruction. We also employ MRI to look at the septal and subvalvular anatomy.
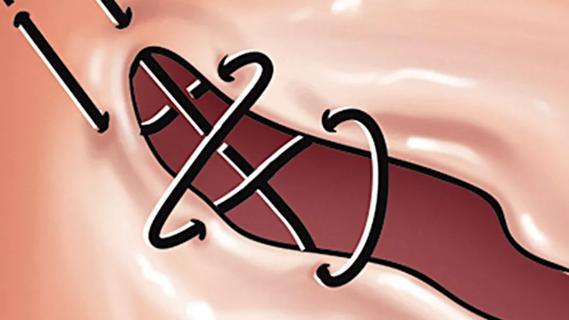
Once LVOTO is documented and the anatomy defined, we consider which surgical options can be used to eliminate the obstruction. While valve replacement can effectively address all cases of LVOTO caused by systolic anterior motion of the mitral valve, we favor repair techniques that avoid prosthetic valve replacement — especially in young, healthy patients.
The surgical options we use include:
In our experience, about 75 percent of patients who have severe LVOTO with minimal or no LV hypertrophy are candidates for corrective repair that avoids valve replacement.
Advertisement
The following composite case vignette illustrates some of the approaches used by surgeons in Cleveland Clinic’s Department of Thoracic and Cardiovascular Surgery when a patient presents with symptoms of LVOTO and minimal septal hypertrophy.
Advertisement

Figure. MRI of a patient with severe obstruction with minimal septal hypertrophy.
Dr. Smedira is a surgeon in the Department of Thoracic and Cardiovascular Surgery. Contact him at smedirn@ccf.org.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
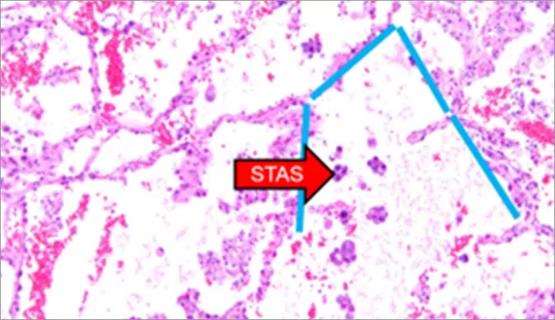
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable