Novel protocol combines gait testing during stimulation with neural signal measurement
Gait impairment is a crucial unmet need for patients with Parkinson’s disease (PD). While deep brain stimulation (DBS) has been studied to treat it, success has been elusive: use of high frequencies can manage some motor symptoms, but can worsen gait, whereas low frequencies may improve gait, but only transiently.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A new feasibility study by Cleveland Clinic researchers — ENGAGE-PD (NCT05022147) — suggests that alternating the frequency of DBS may simultaneously control multiple motor symptoms, including gait. Preliminary results of the research, which involves an experimental paradigm that is being tested in a small group of patients, were presented at the XVII World Congress on Parkinson’s Disease and Related Disorders in early May.
“Our hypothesis is that with an alternating-frequency protocol, patients get the benefit of low frequencies for gait and high frequencies for control of other motor symptoms,” says the study’s first author, James Liao, MD, PhD, a movement disorders clinical fellow in Cleveland Clinic’s Center for Neurological Restoration. “We’ve tested six patients so far using a single-day, 12-condition protocol. In the data analyzed to date, the majority of participants had their most stable gait using alternating-frequency DBS, not the traditional high-frequency DBS.”
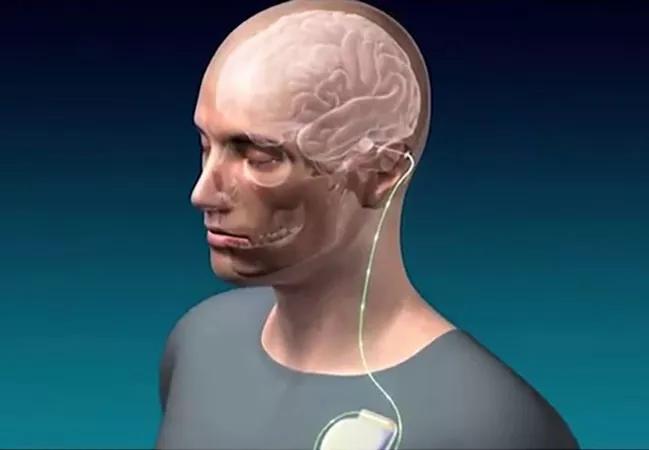
The protocol for the study, which is ongoing, calls for patients with PD and a Medtronic Percept™ DBS system to perform a five-minute gait test while wearing a wireless headset that displays an augmented-reality obstacle course. Participants perform this gait test under six DBS frequency conditions, in random order:
The six tests are performed after holding PD medications and then repeated after taking PD medications, for a total of 12 tests. Short duration is 10 seconds, and long duration is 50 seconds. Low frequency is 55 to 60 Hz, and high frequency is 125 to 130 Hz. A two-minute rest tremor assessment is performed after each test condition.
Advertisement
“As patients go through the obstacle course, we use wearable sensors to assess the stability of their gait,” says Dr. Liao. “Then while they are seated between the walking periods, we’re also measuring tremor.”
In addition, neural data are recorded during the tests. EEG signals are captured with an ambulatory EEG system, and subthalamic nucleus local field potentials are recorded with the Percept neurostimulator.
With the technology involved, gait-related electrophysiology and kinematics can be captured simultaneously and motion/stimulation-related artifact can be mitigated offline. The goals of the study — the first to combine investigation of alternating-frequency DBS with measurement of neural signals — are to identify alternating-frequency strategies that maximize motor benefits and to gain insight into the mechanism of alternating-frequency DBS.
“By analyzing neural data during walking,” Dr. Liao explains, “we hope to figure out how brain activity changes when gait becomes unstable and also learn how DBS modulates brain activity to improve gait.”
All study participants have balance or walking impairment and are able to walk without assistance while off medication. The six patients tested so far on the augmented-reality obstacle course have tolerated the experience, providing support for the feasibility and safety of the approach.
“Our preliminary data show that, in most cases, traditional high-frequency DBS at 125 to 130 Hz isn’t the best DBS condition for gait stability,” notes Dr. Liao. “That’s interesting because it suggests we may be able to improve gait in patients with PD just by adjusting the stimulation frequency.”
Advertisement
Recruitment for the study is ongoing, and the researchers hope to gather additional data in order to draw conclusions about how to best utilize alternating-frequency DBS. “Our ultimate goal is to develop reliable treatments for gait instability and to improve quality of life for our patients without losing the gains they currently enjoy with traditional DBS programming,” says co-investigator Hubert H. Fernandez, MD, Director of Cleveland Clinic’s Center for Neurological Restoration.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade