Research has public health implications

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Metabolic syndrome, or insulin-resistance syndrome, is defined as the presence of hyperglycemia, hypertriglyceridemia, low HDL cholesterol levels, abdominal obesity and hypertension. It affects 23 percent of the U.S. population. Eleven percent of the U.S. population has some form of chronic kidney disease (CKD), and 6 percent has both CKD and metabolic syndrome.
These numbers are increasing secondary to the diabetic epidemic and the growing prevalence of obesity. Patients with metabolic syndrome have higher cardiovascular and all-cause mortality rates. Furthermore, CKD is an independent risk factor for cardiovascular and all-cause mortality, and 50 percent of these patients die of cardiac disease.
We hypothesized that the presence of metabolic syndrome is associated with an increased incidence of end-stage renal disease (ESRD) and death among those with Stage 3 and 4 CKD, and that these associations might be modified by age, gender, race and stage of kidney disease.
To test these hypotheses, we examined the associations between metabolic syndrome, ESRD and death among those with Stage 3 and 4 CKD followed in Cleveland Clinic’s healthcare system.
Of 43,546 patients in our Cleveland Clinic CKD registry (as of Sept. 15, 2009), 25,868 patients (59 percent) had relevant data relating to the different components of metabolic syndrome and were included in this analysis. About 60 percent of the study population (n = 15,605) had metabolic syndrome.
Among these patients, during a median follow-up of 2.4 years (mean 2.3 years), 3,345 participants died before ESRD, and 481 reached ESRD. Overall (pre- and post-ESRD), 3,504 patients died.
Advertisement
The Kaplan-Meier and competing risk analyses showed no significant difference in overall mortality between those with and without metabolic syndrome. However, there were significantly higher rates of ESRD among those with metabolic syndrome than those without metabolic syndrome in both Kaplan-Meier and competing risk analyses (log rank p < 0.001), and the results were similar in both analyses.
In the Cox proportional hazards model, after adjusting for demographic factors, comorbidities, laboratory parameters and kidney function, the presence of metabolic syndrome was not associated with pre-ESRD death. However, the presence of metabolic syndrome was associated with a 33 percent increased hazard for ESRD. An analysis of covariate-adjusted overall mortality (pre- and post-ESRD) provided similar results to that which included only pre-ESRD death, with a hazard ratio (HR) for patients having metabolic syndrome of 1.06 (95 percent confidence interval [CI] 0.98-1.13).
Among the individual components of metabolic syndrome, elevated serum triglycerides (HR 1.07, 95 percent CI 1.00-1.15), impaired glucose metabolism (HR 1.67, 95 percent CI 1.36-2.0) and hypertension (HR 1.83, 95 percent CI 1.04-3.25) were associated with an increased risk for ESRD. Diabetes (HR 1.18, 95 percent CI 1.10-1.27) and low HDL cholesterol (HR 1.10, 95 percent CI 1.02-1.18) were associated with an increased hazard for death, but obesity was associated with a lower hazard for death.
These findings have significant clinical importance, as there is a rapid increase in the individual components of metabolic syndrome, metabolic syndrome itself and CKD in the U.S. population and around the globe.
Advertisement
Metabolic syndrome is widely prevalent in those with nondialysis-dependent CKD, and this has public health implications. Metabolic syndrome is associated with ESRD but not mortality in a diverse population with CKD. The associations between the individual components of metabolic syndrome and outcomes varied, demonstrating a need for further investigation into the mechanisms.
Long-term studies are needed to examine the relationship between metabolic syndrome and mortality in CKD patients. Additionally, whether interventions such as lifestyle modifications can improve the risk associated with metabolic syndrome on kidney disease progression in these patients warrants further study.
At Cleveland Clinic we are conducting additional studies (both observational and interventional) to address these unanswered questions.
Dr. Navaneethan is a staff member of the Department of Nephrology and Hypertension in Cleveland Clinic’s Glickman Urological & Kidney Institute.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
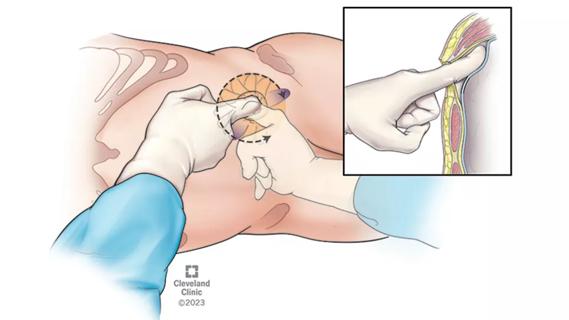
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
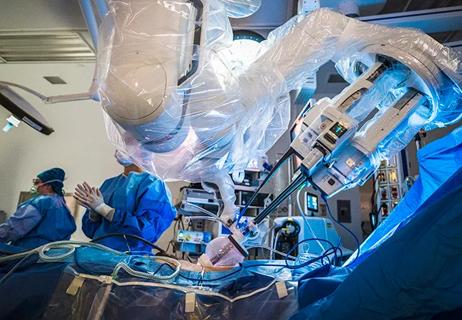
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients