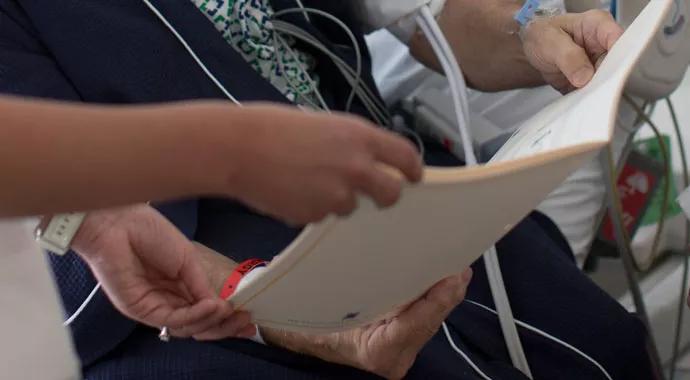
The focus is on heart failure self-care education
How comfortable are nurses at providing heart failure self-care education to patients? That’s what Nancy Albert, PhD, CCNS, CHFN, CCRN, NE-BC, FAAN, and five other nurses sought to discover in a research study. Dr. Albert, who is associate chief nursing officer of Research and Innovation at Cleveland Clinic, served as principal investigator on the multicenter study. Research was guided by three primary questions:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nurses are the primary educators of home-going care for patients hospitalized with chronic medical conditions, such as heart failure. Clinical nurses are expected to provide pre-discharge heart failure education in eight content areas: what heart failure means, medications, diet, activity, weight monitoring, fluid restriction, signs/symptoms of a worsening condition and signs/symptoms of fluid overload.
Dr. Albert and her peers created and implemented a questionnaire for nurses at three hospitals to gauge their comfort in and frequency of delivering pre-discharge education. All 119 participants were registered nurses on short stay, cardiac telemetry, coronary care and heart failure units who had at least six months of experience on their current unit. The questionnaire was divided into three sections:
Nearly 80 percent of participating nurses indicated they were comfortable or very comfortable educating patients about heart failure self-care. Yet nurses generally spent less than 15 minutes educating patients, which is not enough time to assess patients’ needs, provide education and ensure they understand recommendations.
Advertisement
When specific education areas were analyzed, data yielded interesting findings. “The three most important factors in self-care – the ones most likely to stabilize or improve a patient’s clinical status – were the ones that nurses were most likely not to discuss,” says Dr. Albert. These included medications, low sodium diet, and activity and exercise.
These findings point to the importance of educating nurses so they can, in turn, educate patients, says Dr. Albert. It’s imperative that nurses remain abreast of best practices and changes in heart failure self-care principles. For example, two new drugs have recently been released that reduce hospitalization in patients with heart failure – sacubitril/valsartan (EntrestoTM, a replacement for an ACE inhibitor or angiotensin receptor blocker) and ivabradine (Corlanor®, a niche medication used in patients with fast heart rates).
Nurses need to be knowledgeable so they can explain medication actions, side effects, how and when to take them, and what to do if a dose is missed. In addition, some nurses may be unaware of changes in the 2013 ACCF/AHA Guidelines for the Management of Heart Failure regarding the daily limit of sodium intake. It is now individualized to patient needs, rather than making a general statement to limit sodium intake to no more than 2,000 milligrams daily.
“Since nurses are expected to provide patient education before discharge, and patient’s understanding of heart failure self-care may be the basis for adherence to self-care recommendations after discharge, it is important to ensure nurses receive ongoing education,” says Dr. Albert. “It’s also important to develop and implement interventions that ensure patients receive the information they need.”
Advertisement
Complete findings of the research were published in the October 2015 issue of the European Journal of Cardiovascular Nursing in the article “Hospital nurses’ comfort in and frequency of delivering heart failure self-care education.”
Photos ©Russell Lee
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable