Large cohort study finds much lower stroke rate than recent database analyses
The risk of stroke in patients with confirmed retinal artery occlusion (RAO) appears to be lower than previously reported and similar to that in studies of at-risk adults in the general population. So concludes a retrospective study of a large cohort of patients diagnosed with RAO at Cleveland Clinic recently published in the Journal of Vascular Surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings may prompt scrutiny of current American Academy of Ophthalmology guideline recommendations for RAO management that call for urgent evaluation with referral to a stroke center.
“Traditional dogma has been that patients who present with RAO need prompt workup for potential carotid disease and required treatment,” says the study’s corresponding author, Cleveland Clinic vascular surgeon Francis Caputo, MD. “Our study shows that the risk of stroke after a confirmed episode of retinal artery occlusion is very low — less than 1% when concurrent ischemic events are excluded. These findings suggest that recent database studies overestimate the risk of stroke in patients with retinal artery occlusion.”
Large randomized trials support carotid intervention — endarterectomy or stenting — for curbing stroke risk in patients with significant symptomatic carotid artery stenosis, but these trials did not address RAO because of the condition’s low incidence. It develops in about 1 to 2 of every 100,000 persons.
“This creates a dilemma for vascular surgeons when we advise patients on future stroke risk and whether or not to intervene,” notes Dr. Caputo.
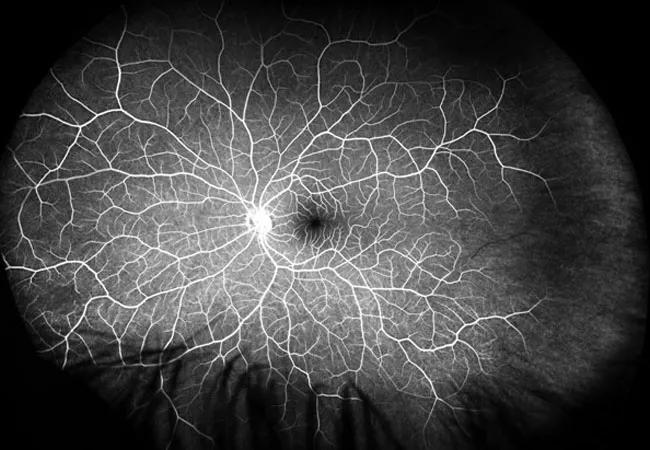
In response, he and colleagues analyzed demographic and clinical data for all patients diagnosed with RAO at Cleveland Clinic from 2004 to 2018. For patients to be included in the analysis, their RAO diagnosis had to be confirmed by fluorescein angiography and they had to be free of known vasculitis.
“These were patients with classic acute, painless loss of vision without resolution and with imaging evidence confirming retinal artery occlusion,” says co-author Alex Yuan, MD, PhD, an ophthalmologist with Cleveland Clinic’s Cole Eye Institute.
Advertisement
A total of 221 patients were eligible for inclusion. Mean age was 66.1 years, and 29% of patients were diabetic. The primary composite endpoint was time to stroke, myocardial infarction (MI) or death over median follow-up of 2.2 years.
Key results included the following:
Carotid artery imaging was available for 141 patients (63.8%), of whom 20 (14.2%) were shown to have >50% carotid artery stenosis. Carotid artery intervention was performed in 10 patients in the cohort, with no strokes reported after these interventions.
Notably, all five patients who had strokes underwent carotid artery imaging, but only one (who had stroke concurrent with RAO) was found to have >50% stenosis of the ipsilateral carotid artery.
“This analysis appears to be the largest study of stroke risk in a cohort of patients with RAO outside of large, nationwide database studies,” says David Laczynski, MD, a Cleveland Clinic vascular surgery resident and lead author of the study. He and his co-authors point out that the nationwide database studies reported to date have been conducted in racially and ethnically homogeneous populations (in Taiwan and Korea) and are limited by an increased propensity for misclassification of RAO and an inability to exclude patients with chronic or asymptomatic RAO.
Advertisement
“We found that stroke risk after confirmed retinal artery occlusion is very low — lower than the 15% to 20% reported in recent nationwide database studies,” notes Dr. Yuan. “However, there are limitations to our study as well. Patients without fluorescein angiography but with clinically confirmed RAO were excluded.”
“The association of ocular findings with stroke risk in the context of carotid artery stenosis has been uncertain,” says Dr. Caputo. “While our findings do not dispute the notion that RAO in the setting of a critical lesion is an indication for intervention, they signal a need for further investigations of risks and best practices in patients with this presentation.”
“We call on other institutions to publish analyses of their own experience with this population to better define stroke risk in this setting, which may help refine management recommendations,” adds study co-author Sean Lyden, MD, Chair of Vascular Surgery at Cleveland Clinic.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable