Teens often require more aggressive care than adults

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/79049e1d-6158-4b32-98f3-99c56bc7ab7a/14-OrT-979-Saluan-Hero-Image-690x380pxl_jpg)
14-OrT-979-Saluan-Hero-Image-690x380pxl
By Joseph Styron, MD, PhD, and Paul Saluan, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The shoulder’s remarkable range of motion has the unfortunate downside of decreased stability since it relies predominantly on soft tissue for restraint. Most shoulder dislocations occur in the second or sixth decades of life, but a shoulder dislocation follows a very different clinical course in a teenager than it does in an adult in his or her 50s.
Young people are more likely to suffer intracapsular dislocations that result in capsular and labral detachments (Figure 1). This injury pattern may partly explain why young patients are far more likely to have subsequent dislocations. At the same time, younger patients are much less likely than their older counterparts to have rotator cuff tears resulting from the shoulder dislocation.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d941b37d-5854-4195-8ee1-525df49f2820/15-ORT-979-Saluan-Inset-Image-Fig-01-590pxl-width_jpg)
Figure 1. Axial cut from an MRI demonstrating an anterior labral tear and posterior bruising of the humerus.
The chance of suffering a recurrent shoulder dislocation is approximately 90 percent in patients under age 20 as compared with approximately 15 percent in patients over age 40. This is believed to be due to the higher type III collagen content in the shoulder capsule and ligaments of teenagers relative to middle-aged adults. Type III collagen is far more supple and elastic than the tougher type I collagen, which is the predominant collagen in the tissues of older adults. This increased elasticity may result in the shoulder capsule and ligaments having too much laxity after a dislocation to provide adequate restraint to keep the glenohumeral joint reduced.
Advertisement
Obtaining a thorough patient history is paramount in determining the cause of the dislocation. In addition, any recurrent sensations of subluxation or instability need to be probed to elucidate the position in which the shoulder feels unstable and the nature of the sensation. Not all patients with shoulders capable of subluxating actually report the sensation, however. In one study, only 50 percent of patients whose shoulder subluxated could feel the sensation of the subluxation.1
The following are among the physical exam signs and tests that can yield findings most consistent with a shoulder with recurrent instability:
Advertisement
Due to the higher risk of recurrent instability in adolescents, particularly among athletes, adolescents with shoulder dislocations may require more aggressive treatment than do older patients. Some studies have demonstrated superior results for operative treatment over nonoperative management in this younger age group. In one study, 75 percent of nonoperatively managed patients developed recurrent shoulder dislocation while only 11 percent of surgically treated patients had recurrent shoulder instability.2
Cleveland Cleveland’s Department of Orthopaedic Surgery has a team of sports health orthopaedic surgeons who provide surgical management of shoulder dislocation in adolescent athletes and bring experience in the subtle differences in management from the adult setting. This team welcomes any patient who has experienced a shoulder dislocation, whether for the first time or on multiple occasions, and will counsel the patient and his or her family comprehensively on the prognosis and treatment options.
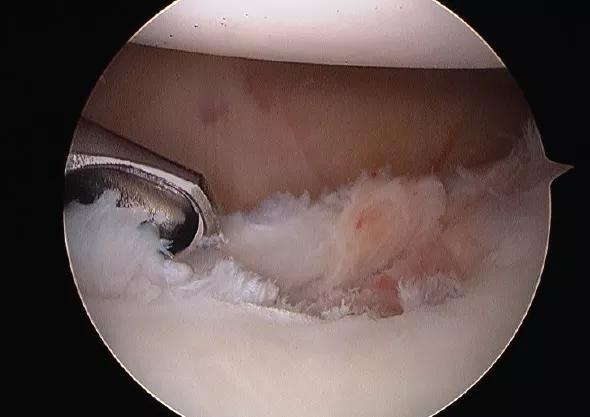
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9a474f23-84ea-4ab6-9826-c81835b3608e/14-ORT-979-Saluan-Inset-Image-Fig-02-590pxl-widthq1_jpg)
Figure 2. Arthroscopic photo of the debridement of the labral tear from Figure 1.
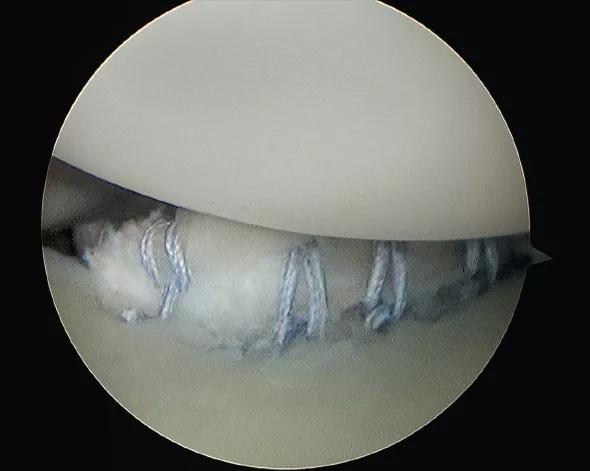
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1930541b-a296-40d0-9587-a7751bae7b29/14-ORT-979-Saluan-Inset-Image-03-590pxl-width_jpg)
Figure 3. Arthroscopic photo of the suture anchors tying down the labrum to the glenoid rim (photo bottom) to restore stability to the glenohumeral joint. (The humeral head is the white dome at the top of the image.)
Advertisement
Dr. Styron is a resident in the Department of Orthopaedic Surgery.
Dr. Saluan is a surgeon with the Center for Pediatric Orthopaedics and Center for Sports Health in the Department of Orthopaedic Surgery.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions