SEEG may aid understanding of psychiatric disorders
By John T. Gale, PhD, and Jorgé Gonzalez-Martinez, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The neural mechanisms that underlie psychiatric disorders are difficult to understand, due to the lack of animal models that adequately represent psychiatric disease states and limitations in the investigational tools available to study human populations.
Cleveland Clinic’s Department of Psychiatry and the Epilepsy Center have recently undertaken a series of behavioral and electrophysiological experiments in patients undergoing evaluation of their seizure disorder. The aim of these experiments is to directly measure the neural control of cognitive processes using an invasive electrophysiological method known as stereoelectroencephalography (SEEG) that can simultaneously record electrical activity from many parts of the brain at high temporal resolution (~1 ms).
These experiments are expected to provide significant insight into mechanisms that underlie psychiatric disease. They avoid using animal experiments that are difficult to interpret and instead employ leading-edge electrophysiological methods for assessing brain function.
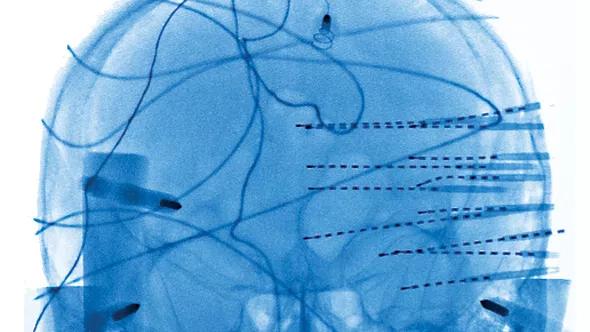
In these seizure disorder patients, many SEEG electrode contacts (as many as 200) are placed directly into the brain to define the area responsible for disease. This methodology has been pioneered in the United States by one of us (Dr. Gonzalez-Martinez) and uses advanced imaging methods in coordination with stereotactic techniques to precisely map the cortical areas responsible for generation and propagation of epileptic activity.
The SEEG method involves rigorous preimplantation scrutiny of all available findings from the noninvasive phase to define the likely location of the epileptogenic zone. The implantation strategy is based on the respective weight of MRI, interictal/ictal EEG and ictal clinical characteristics, which may vary greatly from patient to patient.
Advertisement
After formulating an individualized hypothesis about the epileptogenic zone’s location, physicians plan a tailored SEEG implantation strategy with the goal of confirming or rejecting the hypothesis. The precision of the stereotactic technique allows the desired targets to be reached and recorded from lateral, intermediate or deep structures in a three-dimensional arrangement, thus accounting for the dynamic, multidirectional spatiotemporal organization of the ictal discharges (Figure 1).
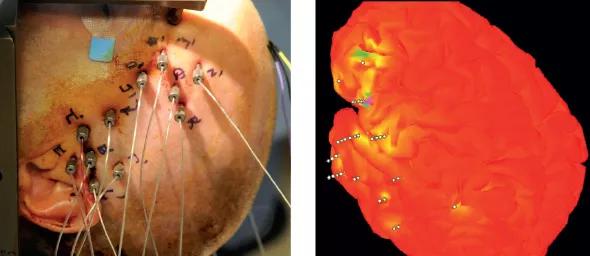
Figure 1. Patient in stereotactic frame with SEEG recording electrodes in place (left); three-dimensional model (right) shows brain region activation during phases of the card game. The 3-D image was constructed with Brainstorm Image reconstruction software. (See: Tadel F et al. Brainstorm: A User-friendly Application for MEG/EEG Analysis. Comput Intell Neurosci vol 2011; 2011:879716.)
Once these contacts are positioned, patients remain in the hospital for as long as three weeks. During this time, we can have patients perform a battery of behavioral tasks designed to probe various aspects of cognition.
While the goal of the SEEG implantation is to define the patients’ seizure disorder, these patients often welcome the opportunity to participate in our research, as it provides them with some level of distraction during their hospitalization. Moreover, this research does not pose additional risk to patients and can be performed in the hospital room, without interfering with the clinical analysis of their epilepsy. Prior to participation, subjects review a consent form outlining the study’s goals and potential risks. The research has been approved by Cleveland Clinic’s Institutional Review Board.
Advertisement
Here we present the results of a behavioral task used to probe the processes of decision-making and reward encoding, two fundamental brain functions thought to be involved in major depression and obsessive compulsive disorders. In this task, patients play a card game against a computer while their brain activity is recorded.
The card game is similar to the child’s game of War. Patients are required to make a financial wager based on their expectation of beating the computer’s card. To make the game simpler for analysis, we limit the cards to even-numbered ones of the same suit (e.g., 2, 4, 6, 8 and 10 of spades). Thus, the 10 card represents the highest odds of winning and the 2 card the lowest, with the 6 card representing a 50 percent chance of winning.
The patient first sees his or her card and the back of the computer’s card. After a brief delay, the patient is asked to make a wager of either $5 or $20, based on the expectation of winning. The patient then is shown the computer’s card, followed by a screen depicting whether the patient’s hand wins or loses.
In a precursory analysis of the SEEG data capture from one patient playing the game, we can demonstrate that various aspects of the task evoke significant gamma-band modulation in the brain. In the visual cortex, the presentation of an object on the screen results in a fast latency (~200 ms) response, regardless of task outcome.
In contrast, the inferior frontal gyrus is modulated only in trials that result in a reward (Figure 2).
Advertisement
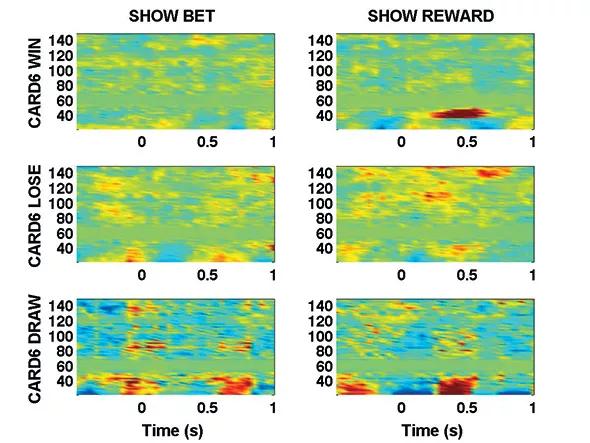
Figure 2. Spectrograms of activity in the inferior frontal gyrus relative to two different epochs (t = 0) in War task. (X axis: Time relative to epoch. Y axis: Frequency. Color represents z-score relative to baseline.)
This modulation is longer in latency (~300 ms), suggesting a period when the reward information is being processed. The reward-related responsiveness is consistent with the function of that part of the cortex, as it is hypothesized that the inferior frontal gyrus is involved in decision making and reward evaluation.
Although preliminary, these data are exciting because they demonstrate that the behavioral task elicits different responses in the brain that are dependent on the patient’s choice.
Functional magnetic resonance imaging has been used to study neural firing patterns during behavioral tasks, but it can resolve global fluctuations only in response to the overall task. The SEEG method is capable of resolving brain activities at scales relevant to the behavior being studied, allowing us to see brain fluctuations related to individual time periods of the task, such as when patients see their card or the outcome of their bet.
Our next goal is to extend our analysis across many more brain regions in patients that we have recorded, to gather a larger picture of how the brain governs decision-making. In the long term, we plan to apply this knowledge to better understand how changes in these parts of the brain contribute to psychiatric disease, and to develop new strategies for treatment.
Advertisement
Dr. Gale is an assistant staff member in Cleveland Clinic’s Center for Neurological Restoration and Department of Neurosciences.
Dr. Gonzalez-Martinez is an associate staff member in the Center for Neurological Restoration.
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade