‘Orchard of Apps’ strategy leverages data elements across neurologic conditions

By various measures, last year was a good one for Cleveland Clinic’s C3Logix™ app:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But the most enduring legacy of C3Logix is likely to be the collection of mobile healthcare apps that Cleveland Clinic’s Neurological Institute has been developing in its wake using selected C3Logix modules and insights from its initial use. These efforts accelerated in 2014 and were formalized into a coordinated strategy — dubbed the “Orchard of Neurological Apps” — to efficiently leverage digital health technology and common data elements across a range of neurologic conditions.
“Instead of using new digital health technologies to create one-off apps, which leads to multiple fragmented approaches to care, we’re looking at mobile apps as modules to be applied across common functional domains for various conditions,” says Cleveland Clinic Concussion Center Director Jay Alberts, PhD, the primary force behind the C3Logix app, which debuted in 2011.
Dr. Alberts took on an additional title in 2014 — Institute Vice Chair for Health Technology Enablement — and was charged with overseeing the Orchard of Neurological Apps strategy.
The essence of the strategy is to use related mobile healthcare apps to develop, implement and test predictive treatment models by collecting objective, quantitative outcomes among populations of patients with various neurologic conditions. By building “big data” outcomes repositories through collection of common data elements across these associated apps, the institute aims to guide refinement of care paths and enable predictive models of care.
“Mobile apps provide an unprecedented means to collect objective and truly mineable outcomes throughout the treatment process,” says Dr. Alberts. They also offer singular opportunities for data visualization.
Advertisement
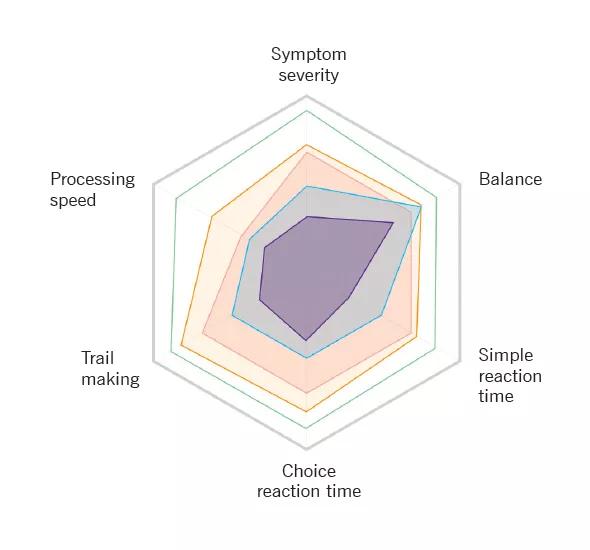
Figure 1. Example (from the multiple sclerosis app) of the data visualization that’s possible across multiple domains of function under the Neurological Institute’s model of mobile app development.
Central to the strategy is the development of a series of assessment modules that quantify domains of functional impairment common to various neurologic conditions. Dr. Alberts cites the example of postural stability. “Patients with multiple sclerosis, Parkinson disease, stroke or concussion all may have balance problems. So there’s no reason to create separate balance tests for each and have fragmented approaches to assessment.”
Accordingly, the C3Logix app’s balance module has been integrated into Neurological Institute apps for multiple sclerosis, Parkinson disease/essential tremor and fall risk assessment. Similar approaches have been taken with other cognitive and motor domains.
Figure 2.
Dr. Alberts foresees the Orchard of Neurological Apps strategy being rolled out in three overlapping phases over the next several years:
Advertisement
Operationally, data from the collection of mobile apps will be used to build an ever-evolving database that will allow providers at Cleveland Clinic and beyond to evaluate patients with these apps and identify the clinical state of their patients relative to others presenting with similar symptoms and dysfunction. The provider can then determine how the patient may respond to various interventions (see figure below), the rate of disease progression and other fundamental aspects of management.
“Coordinated application of these tools can move us from an episodic care model to a patient specific model in which clinical decisions are driven by outcomes from large data sets rather than clinical dogma or the treating physician’s experience base,” says Dr. Alberts. “Our aim is to turn mobile devices from expensive electronic notebooks into data collection systems that can transform the quality and cost of medicine.”
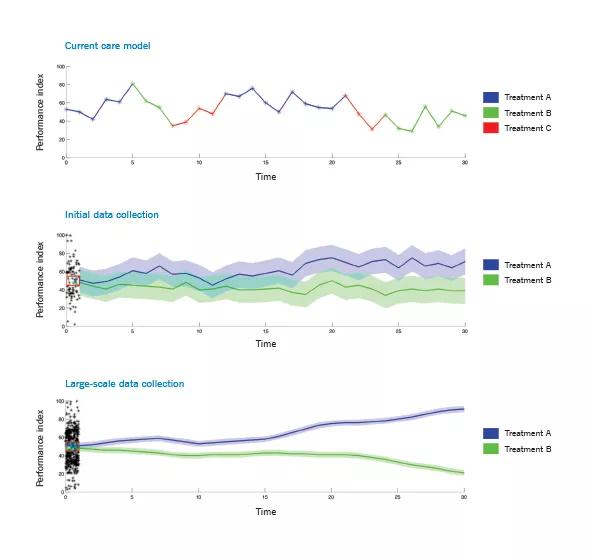
Figure 3. Plots depicting how care may be transformed through predictive analytics for individual patients made possible by the Orchard of Neurological Apps. The top plot represents the current model of care for many neurological patients, with variable outcomes (shown on the y-axis) as different treatments and doses are tried based on response to subjective clinical assessments of cognitive or motor function. The result is time-consuming and costly care that does not optimally serve the patient. The middle plot illustrates the initial value of collecting objective functional outcomes in combination with treatment protocols in a relatively large set of patients (e.g., 1,000). Variability in outcomes over time has been reduced, but the overlap in confidence fields around the plots for Treatments A and B shows some remaining uncertainty about which treatment is best for a patient presenting at a given functional level. The bottom plot shows how clearly distinct outcomes between Treatments A and B might be predicted for a given patient early in management once predictive treatment models are well-populated through large-scale collection (e.g., tens of thousands of patients) of objective outcomes from mobile apps. As the size of the database grows, the predictive modeling has less variability and becomes more patient-specific.
Advertisement
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade