Procedural success tops 99 percent with mortality of 0.1 percent

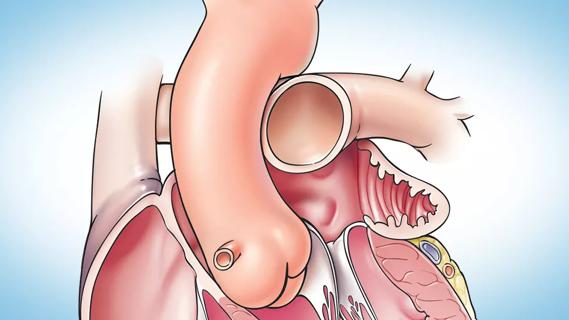
Robotic surgery, the least invasive approach to mitral valve (MV) repair, yields a procedural success rate exceeding 99 percent and operative mortality of just 0.1 percent (1/1,000). So reveals an analysis of the first 1,000 robotically assisted MV surgery cases performed at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Despite reports documenting the safety and efficacy of robotically assisted mitral valve surgery, it has not become the standard of care for managing mitral valve disease,” says the study’s lead author, Cleveland Clinic cardiothoracic surgeon A. Marc Gillinov, MD, who presented the analysis at the American Association for Thoracic Surgery annual meeting in Baltimore on May 18.
“These results may help change that, as we’ve shown that robotic surgery enables mitral valve repair with high procedural success and low risks of morbidity and mortality,” he adds. “Moreover, procedural safety and effectiveness improved with increasing experience and application of algorithm-driven patient selection.”
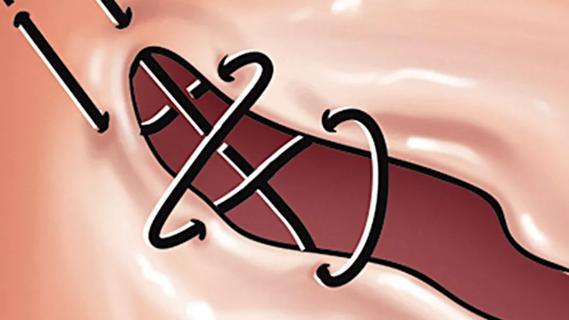
The analysis examined clinical outcomes among 1,000 consecutive patients who underwent primary robotically assisted MV surgery at Cleveland Clinic from January 2006 to November 2013 — 30 percent of the institution’s primary isolated MV surgery cases over that period. Robotically assisted MV surgery was performed with concomitant procedures in 164 cases. All procedures were done via right chest access with femoral perfusion.
Mean patient age was 56 ± 10 years, and etiologies of MV disease were as follows:
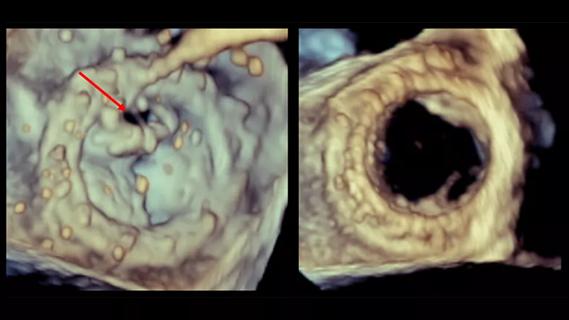
MV repair was attempted in 997 patients, with the remaining three undergoing planned MV replacements (n = 2) or resection of fibroelastoma (n = 1). Of these 997 patients, 992 underwent MV repair and five underwent replacement.
Advertisement
Intraoperative post-repair echo graded mitral regurgitation as mild or less in 99.7 percent of repair patients upon departure from the operating room, and pre-discharge echo confirmed that regurgitation remained mild or less in 97.8 percent.
Other key findings:
After about the first 500 cases in this experience, the surgical team added CT scanning of the chest, abdomen and pelvis to the screening protocol for robotic surgery candidates, to detect peripheral artery disease or atherosclerosis that would contraindicate femoral perfusion. “Preoperative CT scanning identifies patients at risk, enabling use of safer perfusion strategies,” Dr. Gillinov explains. “These might include axillary artery cannulation for cardiopulmonary bypass.”
At this time the team also incorporated all imaging studies into an algorithm to guide patient selection for robotically assisted surgery. “Our algorithm directs patients with unfavorable features to a nonrobotic approach,” says Dr. Gillinov, “which generally provides a safer option for mitral valve surgery in those patients.” The algorithm will be included in the full report of this analysis, which has been submitted for publication.
Dr. Gillinov believes these findings may address lingering reluctance toward adoption of a robotic approach to MV repair, which has stemmed from concerns about prolonged operative time, quality of valve repair and hospital resource use.
Advertisement
“Robotically assisted mitral valve repair is a safe and effective approach for correcting mitral regurgitation, and safety and efficiency improve with experience,” he says. “It has now set a standard for comparison with emerging percutaneous mitral valve interventions.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
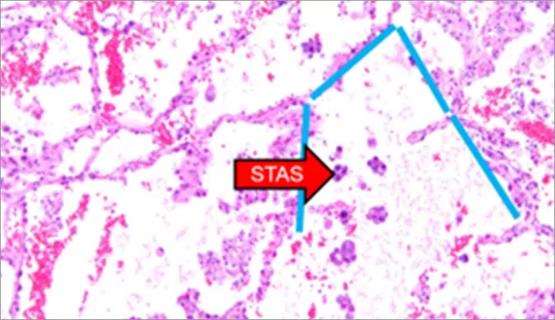
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
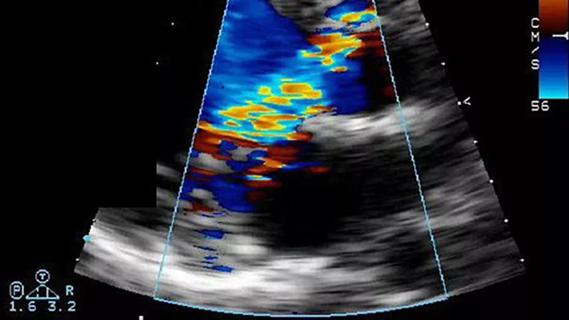
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable