An affiliated health system reflects on working with Cleveland Clinic

As detailed previously on Consult QD, Cleveland Clinic’s Miller Family Heart & Vascular Institute has built a network of affiliated and allied provider organizations across the U.S. to share best practices and help these organizations enhance their cardiovascular programs from clinical, operational and strategic perspectives. This post profiles how Cleveland Clinic’s relationship with one such affiliate, CHRISTUS St. Michael Health System, helped that organization revamp several aspects of its cardiac surgery registry — and improve outcomes in the process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In January 2014, Cleveland Clinic formed a cardiovascular surgery and cardiology affiliation with CHRISTUS St. Michael Health System, a Catholic health system and part of CHRISTUS Health, which has served the Texarkana region of Arkansas, Texas, Louisiana and Oklahoma since 1916. The relationship evolved from a consulting agreement that began in 2012.
At the start of the affiliation, the two institutions identified an opportunity to enhance feedback on quality and improve mortality and morbidity outcomes among cardiovascular surgery patients. CHRISTUS St. Michael enjoys strong physician and administrative engagement and leadership, yet key stakeholders questioned the validity of registry data for the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database, which created an environment of mistrust around reported cardiovascular outcomes.
As a result, this high-functioning, patient-focused cardiovascular program was experiencing less-than-desirable outcomes because it lacked adequate processes to accurately collect, validate, analyze and communicate results across clinical disciplines to engage physicians in quality improvement.
CHRISTUS St. Michael’s physician leaders and administrators worked with Cleveland Clinic’s affiliate program team to identify key obstacles to improving surgical outcomes and feedback on quality metrics, and they developed strategies to overcome them, as outlined below.
Advertisement
Under the leadership of Regional Chief Medical Officer Mike Finley, MD, as well as cardiothoracic surgeon Michael Cannon, MD, and the CHRISTUS St. Michael administrative team, these changes have brought about the following:
• Improved data collection and validation
• Improved transparency of STS outcomes data among physicians
• Greater physician trust
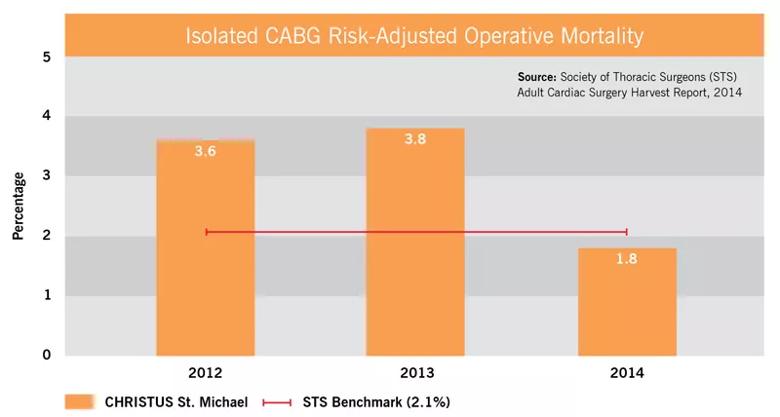
Notably, they’ve also brought about a substantial improvement in CHRISTUS St. Michael’s coronary artery bypass graft surgery (CABG) mortality for 2014 relative to the two prior years and to the STS benchmark, as detailed in the graph below. The observed-to-expected mortality ratio for 2014 (0.89) was likewise substantially improved from the ratios for 2012 (1.78) and 2013 (1.91).
In addition to improved data quality and transparency and greater physician trust, two other factors likely help explain this improvement in mortality:
• A concentrated emphasis on preoperative risk assessment and determination of appropriateness and timing of surgery
• Greater appreciation of the need to consider referring patients deemed high-risk (based on STS preoperative risk score or clinical judgment) to a major facility for surgery
“This affiliation has allowed our physicians to have real-time consultation with our partners at Cleveland Clinic,” says Dr. Finley. “Cases are discussed and studies are reviewed, sometimes with multiple physicians. This collaboration has provided our physicians with input and confidence when making decisions about treatment options and patient selection, which has been invaluable to patient care.
Advertisement
“Just as important has been the opportunity to validate and improve our data collection so that it accurately reflects our patient experience,” Dr. Finley adds. “Our surgical team has benefited greatly from Cleveland Clinic’s site visits, the processes we’ve implemented have been highly successful, and the assistance in strategically evaluating new technology and services has been extremely helpful. We could not be more pleased with this affiliation.”
For another post in this series profiling how Cleveland Clinic’s Miller Family Heart & Vascular Institute has collaborated with its allied and affiliated provider organizations — this time MedStar Heart & Vascular Institute — click here.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable