Characterization could aid communication and outcome prediction

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some renal tumors have a size or location that requires the resection of a significant portion of the renal parenchyma during a partial nephrectomy. Resection of approximately half the kidney in these complex cases is sometimes referred to as a heminephrectomy. The term is most commonly used when more than 30 percent of the renal mass is removed.
A definition relying only on the amount of tissue excised, however, does not properly classify those procedures during which a large interpolar mass or an extensive exophytic mass is resected.
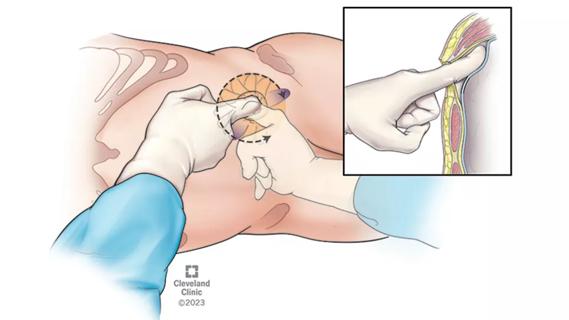
Based on the following analysis, we propose a specific definition of heminephrectomy: Excision of the upper or lower pole of the kidney, removing at least 30 percent of the parenchymal mass, cutting to hilar fat and transecting the collecting system.
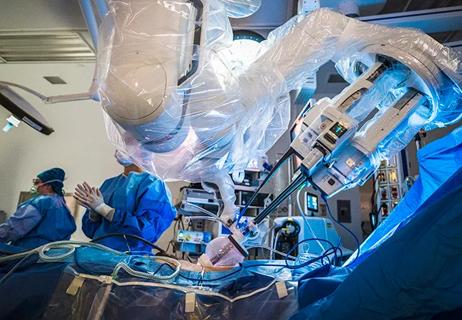
We queried our Institutional Review Board-approved database for those patients who underwent robotic or laparoscopic partial nephrectomy between 2002 and 2011 with resection of at least 30 percent of the renal parenchymal mass, exposure of hilar fat in the resection bed and opening of the renal collecting system.
For purposes of determining the percentage of the kidney resected, we defined total parenchymal mass as the volume of the tumor plus the volume of the affected kidney. The percentage of renal parenchymal mass removed was estimated by the surgeon based on intraoperative findings and preoperative CT scan.
We compared patients who underwent a robotic or laparoscopic heminephrectomy with the remainder of patients who had a robotic or laparoscopic partial nephrectomy. To reduce confusion, we excluded patients who had a “true” heminephrectomy for obstruction in a duplicated collecting system. We also excluded patients with resection of half of a horseshoe kidney.
Advertisement
Sixty-one of 643 patients who underwent a minimally invasive partial nephrectomy for tumor during the study period met our definition of heminephrectomy. Of the heminephrectomies, 16 (26 percent) were performed laparoscopically and 45 (74 percent) were performed robotically, while 200 (34 percent) of the nonheminephrectomy partial nephrectomies were performed laparoscopically and 382 (66 percent) were performed robotically.
Table 1 summarizes the patient characteristics and comparative outcomes. The tumors in the heminephrectomy group were larger (5.1 cm vs. 2.8 cm, p < 0.001) and had a higher RENAL score (8.5 vs. 6.5, p < 0.001). Estimated blood loss was greater (373 mL vs. 267 mL, p = 0.04), operative time was longer (214 minutes vs. 185 minutes, p < 0.001), warm ischemia time was longer (25 minutes vs. 20 minutes, p = 0.002), the rate of intraoperative complications was greater (5 [8 percent] vs. 15 [3 percent], p = 0.02), and the rate of conversion to radical nephrectomy was greater (4 [7 percent] vs. 1 [0.2 percent], p < 0.001) in the heminephrectomy group.
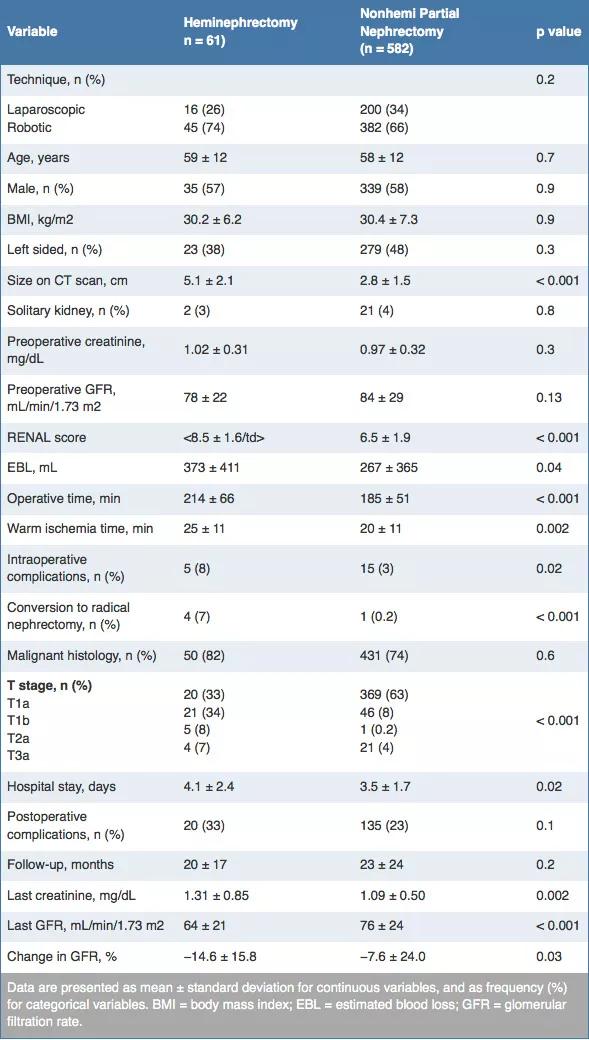
Table 1. Heminephrectomy vs. nonheminephrectomy minimally invasive partial nephrectomy
Length of hospital stay was slightly longer in the heminephrectomy group (4.1 days vs. 3.5 days, p = 0.02). The decrease in glomerular filtration rate (GFR) from preoperative to most recent value was greater (mean −14.6 mL/min/1.73m2 vs. −7.6 mL/min/1.73m2, p = 0.03) in the heminephrectomy group. On multivariable analysis adjusted for age, preoperative GFR, RENAL score and warm ischemia time, heminephrectomy was a significant predictor of lower postoperative GFR (p < 0.001) and of greater decrease in GFR from preoperative to most recent GFR (p < 0.001).
Advertisement
Patients undergoing robotic vs. laparoscopic heminephrectomy were significantly more likely to have more comorbidities (Charlson index 3.4 vs. 1.4, p < 0.001), larger tumor size (5.6 cm vs. 3.7 cm, p = 0.002) and higher RENAL score (8.9 vs. 7.4, p < 0.001). Despite these factors — all of which make heminephrectomy significantly more difficult — the operative times, warm ischemia times and estimated blood loss were similar between the robotic and the laparoscopic heminephrectomy groups (Table 2).
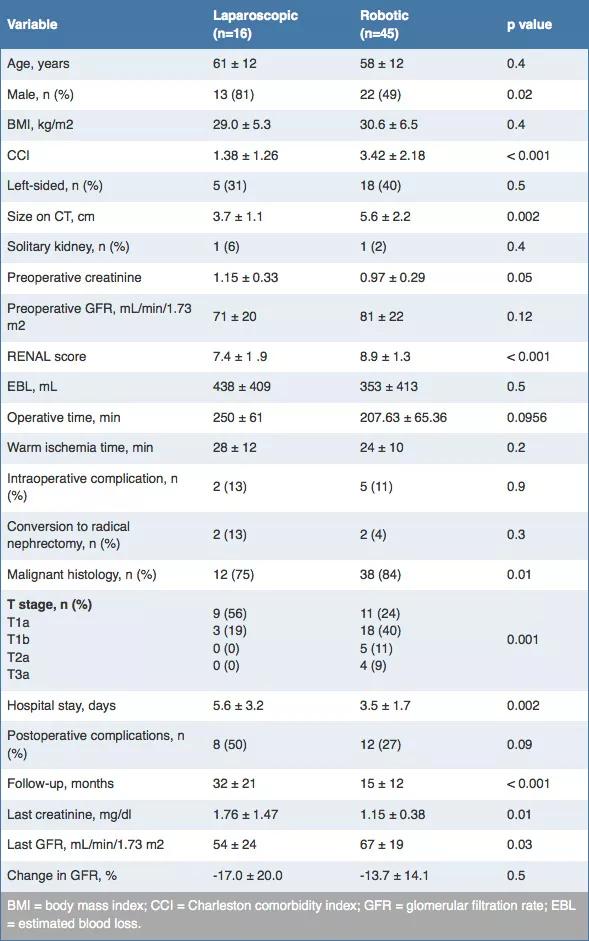
Table 2. Laparoscopic vs. robotic heminephrectomy: patient characteristics and operative outcomes
Chronic kidney disease (CKD) upstaging occurred after heminephrectomy in 30 patients (49 percent) and never exceeded a one-stage increase. New-onset renal insufficiency (CKD Stage 3 or higher) developed in 12 patients (20 percent). No patient progressed to dialysis dependence.
In conclusion, this analysis shows that a heminephrectomy performed for tumor in a nonduplicated system may be defined by excision of the upper or lower pole of the kidney, removing at least 30 percent of the parenchymal mass, cutting to hilar fat and transecting the collecting system.
This definition might allow precise clinical and research communication about heminephrectomy patients and may aid in the prediction of outcomes after partial nephrectomy. Robotic heminephrectomy is a safe and effective method to remove large renal polar masses.
Dr. Kaouk is Director of Cleveland Clinic Glickman Urological & Kidney Institute’s Center for Robotic and Laparoscopic Surgery and is the Urological & Kidney Institute’s Vice Chair for Surgical Innovations. He is a Professor of Surgery at Cleveland Clinic Lerner College of Medicine.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
Pioneering and refining the approach in pyeloplasty, nephrectomy and more
Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients