Will use machine learning and more to gauge survival disparities
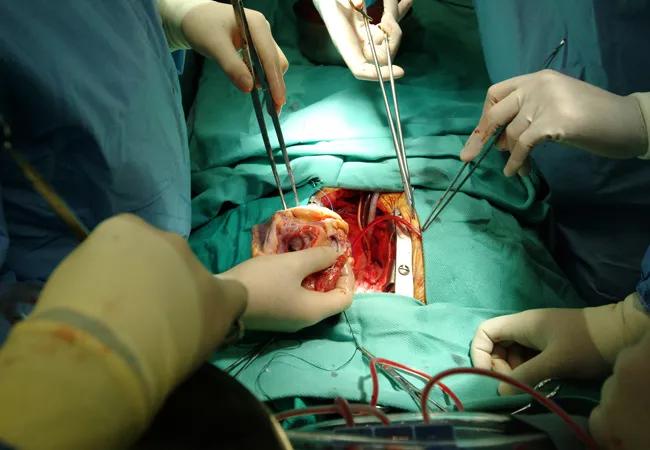
The National Institutes of Health has awarded a research team led by Cleveland Clinic cardiologist Eileen Hsich, MD, $2.8 million to examine disparities in survival among heart failure patients before and after heart transplantation. The four-year grant also supports development of new data tools, including machine learning methods, to optimize outcomes in this population.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Disparities in survival exist among patients during their time on the waiting list for heart transplant and also following transplantation,” says Dr. Hsich, Associate Medical Director of Cleveland Clinic’s Cardiac Transplant Program and co-principal investigator (PI) on the grant. “The research funded by this award will identify factors contributing to these population differences, with the aim of improving survival and minimizing organ wastage.”
She adds that the goal is to lay the groundwork for ultimate development of “a dynamic and improved way to allocate donor hearts in the future,” although the current grant does not cover work to create an allocation score.
The grant will support three research projects focused on the following:
Advertisement
“The existing heart allocation system is based on tiers that prioritize patients by risk of death mainly by need for mechanical circulatory support or certain medications, but it doesn’t account for how their condition changes, their likelihood of getting transplanted or their risk of death after transplant,” explains Dr. Hsich, who has published extensively on disparities among heart transplant candidates (see this prior Consult QD story).
Dr. Hsich will collaborate closely with her co-PI, Hemant Ishwaran, PhD, Director of Statistical Methodology at the University of Miami Health System, who formerly worked at Cleveland Clinic. She says the statistical models to be developed will be more sophisticated than the dynamic model currently used for liver allocation and should ultimately be applicable to allocation of donor organs beyond the heart.
“Our approach is innovative because it uses new mathematical approaches and seeks to shift current heart failure research and clinical practice paradigms by taking into account population differences rather than basing decisions solely on ejection fraction, presence of coronary artery disease and stages of disease,” Dr. Hsich observes.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable