How we helped an allied hospital keep pace with growing case volumes
Over the course of 2018 and 2019, St. Luke’s Hospital in greater St. Louis, Missouri, saw swift and steady growth in its electrophysiology (EP) program. In little more than a year, the hospital’s two EP labs — each with EP-dedicated nursing/tech staff — went from an average of fewer than 50 cases per month to nearly 100 cases per month (see graph below). The growth exerted stress on the system, creating long days for EP providers, increasing overtime costs and contributing to provider burnout.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
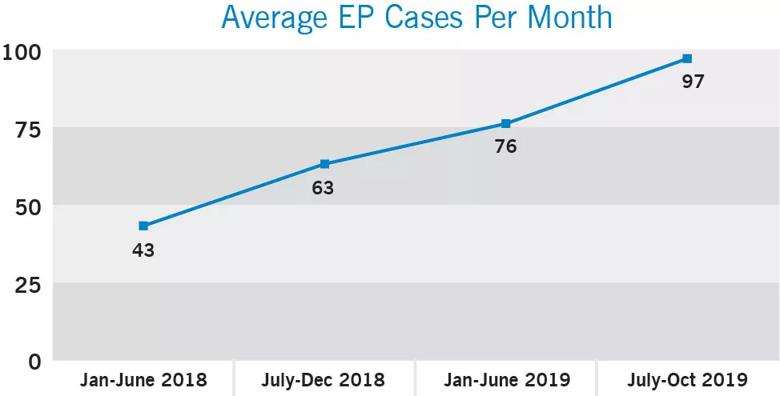
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e2f077a4-679e-44af-8471-926e301200e0/20-HVI-1869562-CQD-Affiliate-Case-Study-charts-1_jpg)
To help meet the increasing demand for EP services while managing these stresses, St. Luke’s turned to its alliance relationship with Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute, which has been in place since 2016 to promote sharing of best practices in clinical care, quality improvement and operational efficiency.
Under the alliance, Cleveland Clinic makes its Continuous Improvement Service (i.e., CI team) available to advise partner organizations on operational challenges. Jeanne Secrest, BSN, RN, nurse manager of St. Luke’s cardiac catheterization and EP laboratories, engaged with this team and Cleveland Clinic’s EP clinical consultant for alliances and affiliations. “Our primary goal was to identify opportunities to enhance the EP labs’ ability to run more efficiently, increase productivity and lower overtime utilization,” says Secrest. “We believed that improvement in these areas would reduce provider burnout as well.”
Cleveland Clinic’s CI team and EP clinical consultant worked with Secrest to establish and track operational efficiency metrics in the EP labs, reviewing the time stamps to be captured for each case, essential key metrics to establish and goals to work toward. This type of data-driven approach increases visibility into daily operations and provides a clear focus on where areas of opportunity exist.
Once refined data collection was underway in response to this review, the CI team used the data gathered by Secrest’s team to perform baseline and updated operational efficiency analyses of the EP labs. The following operational metrics were analyzed:
Advertisement
The baseline efficiency analysis was presented in April 2019 to the nurse manager, EP lab medical director and vice president of St. Luke’s cardiovascular service line. This led to development of a plan to address the opportunities identified through the analysis. The plan and its rationale were presented to physician and nursing staffs to gain buy-in and support of the changes. Opportunities identified included improvements in room turnaround time, first case start times and, most importantly, lab and staffing utilization rates relative to actual caseload.
Prior to completion of the updated efficiency analysis by the CI team in June 2019, EP lab nurses were scheduled for five 8-hour shifts, Monday through Friday, and the EP labs’ operating hours were 8 a.m. to 4 p.m. four days a week. However, because of the increase in case volume — especially the consistent supply of add-on cases late in the day — nursing staff were regularly working 10-hour shifts. This contributed to high rates of overtime and low staff morale. Moreover, some physicians’ EP cases were being scheduled months out, due to the growing volume, daily add-ons and staffing schedule issues.
One focus of the efficiency analysis was how much procedure time was taking place after 4 p.m., the nominal “closing” hour, relative to overall lab utilization. As shown in the graph below, during each of the time periods of volume growth, the labs were between 75% and 80% utilization (which is the goal, in order to leave 20% available for urgent cases or unassigned block time) and grew to consistently have cases until almost 2 hours beyond the primary operating hours.
Advertisement
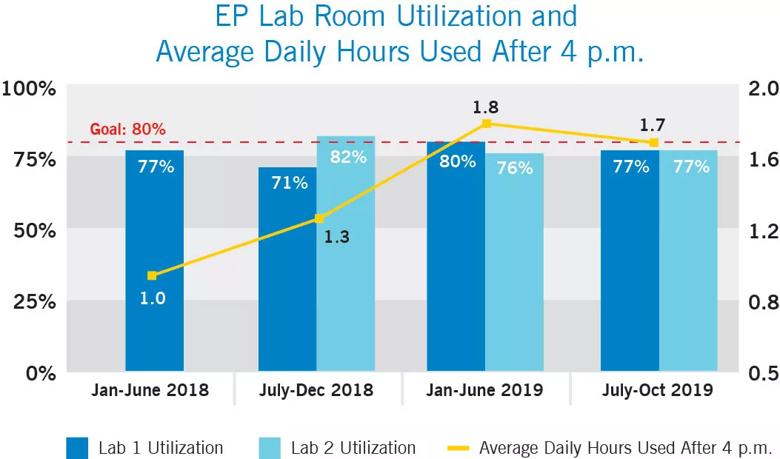
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eb96dbb4-f62e-444f-8df4-f131050631b2/20-HVI-1869562-CQD-Affiliate-Case-Study-charts-2_jpg)
The analysis identified an opportunity to adjust the EP nursing staff’s shifts from 8 hours across 5 days to 10 hours across 4 days to align with the actual length of lab days. This would reduce utilization of overtime and expand the EP labs’ collective available procedure time by 25% weekly.
In July 2019, St. Luke’s EP leadership implemented Cleveland Clinic’s recommendation of four 10-hour shifts, with nurses working 7 a.m. to 5:30 p.m. or until the last case is done. This allowed one EP lab to be fully run five days a week while the second EP lab is staffed three days a week to align with physicians’ scheduled lab and office time.
These changes proved impactful: Over the first six months of moving the nursing staff to the 10-hour shift model, overtime utilization decreased by 44%, reducing the overtime payout by 44% as well. This was achieved even as the total number of FTEs stayed constant (see graph below) and the total individual procedure volume increased slightly.
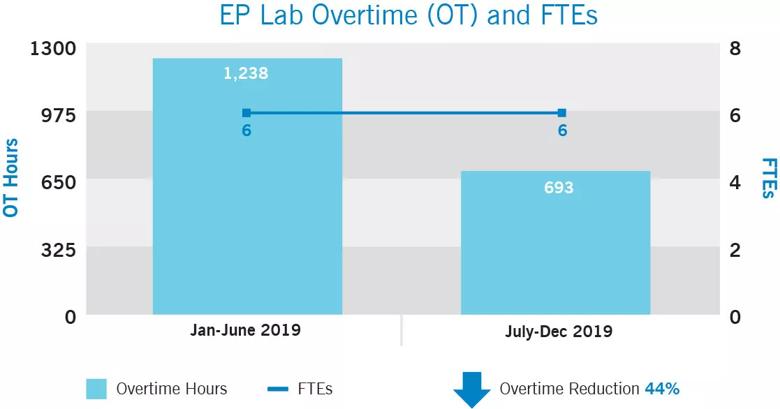
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/39d3c89b-e99a-433c-9f5e-233b17b1cb62/20-HVI-1869562-CQD-Affiliate-Case-Study-charts-3_jpg)
St. Luke’s EP leadership team attributes these significant improvements in operational efficiency to collaboration among the nurse management team, hospital leadership, physicians and Cleveland Clinic’s CI team.
“Everyone had to work together to understand the importance of data collection, time tracking, monitoring efficiency metrics and using data to drive decisions,” says Secrest. “The data analysis provided by the Cleveland Clinic team made clear to us that the day-to-day demands on our team needed to change. The transition to four 10-hour shifts has led to a healthier work-life balance for the EP nursing staff, which has resulted in increased job satisfaction.”
Advertisement
These results prompted the St. Luke’s team to identify further opportunities to streamline the daily workflow in the EP lab setting, promote operational efficiency, improve staff morale, reduce labor costs and improve resource utilization. A second Cleveland Clinic recommendation — a monthly clinical and business review meeting — has been implemented to support these ongoing improvement efforts and enhance the transparency of daily EP lab operations. The monthly meetings are used to discuss quality, efficiency, productivity and cost reduction strategies.
The St. Luke’s EP program will continue to work with Cleveland Clinic’s EP clinical consultant and CI team to support ongoing efficiency efforts, specifically:
For information on affiliation and alliance opportunities with Cleveland Clinic’s Heart, Vascular & Thoracic Institute, visit clevelandclinic.org/heartaffiliates or email HVI_Strategic_Operations@ccf.org.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable