Strong understanding of the abdominal anatomy is key
Ultrasound-guided injection of local anesthetic in the fascial plane offers anesthesiologists a method that is effective and safe with few complications. One relatively new approach in this realm is the quadratus lumborum (QL) block, a variant of the transversus abdominis plane (TAP) block.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over the past four years, Hesham Elsharkawy, MD, staff in the Department of General Anesthesiology, and his colleagues at Cleveland Clinic have extensively studied the QL block. They have developed a specialized approach to performing it and have successfully lobbied for a change in the procedure’s nomenclature. “The QL block has advantages,” Dr. Elsharkawy says, “because you can tailor it to different areas of the body such as the lower chest wall, the upper abdomen, lower abdomen and even the hip and lower extremities.”
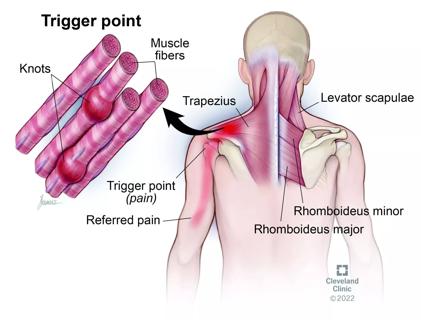
The following illustrations highlight important considerations for physicians performing the QL block. All images are republished with permissions from Elsevier and were originally published in Advances in Anesthesia.

Advertisement




Advertisement


Slide 1/7
Advertisement
Advertisement

Two-hour training helps patients expand skills that return a sense of control

Program enhances cooperation between traditional and non-pharmacologic care

National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS

Pain specialists can play a role in identifying surgical candidates

Individual needs should be matched to technological features

New technologies and tools offer hope for fuller understanding
Pathophysiology, diagnosis, treatment and a COVID-19 connection

Clinical judgment is foundational to appropriately prescribing