Lessons from the care of two face transplant recipients
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
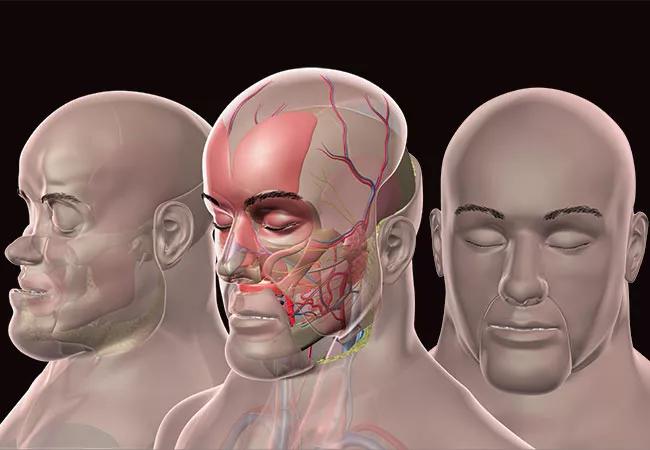
Now that Cleveland Clinic has performed two near-total face transplants, most recently in 2014, we’ve learned a vast amount about how to ensure recipients have favorable outcomes — both physically and psychologically. Face transplant improves not only a patient’s appearance, but also his or her quality of life. It can reverse the negative psychological effects of a traumatic injury, as our group reported in a recent three-year psychological outcomes follow-up on the first patient to undergo a near-total face transplant at Cleveland Clinic.
As a clinical psychiatrist on Cleveland Clinic’s large, multidisciplinary face transplantation team, I work with patients a full year before and a full year after their surgery. Psychiatry plays a vital role in face transplantation, providing patients with support in three broad areas as detailed below.
For months before the surgery, face transplant candidates meet regularly with me for psychiatric evaluation, the essentials of which I reviewed in a recent publication. Along with a transplant coordinator and social worker, we discuss the realities of transplantation, immunosuppression, success rate and risks.
A bioethics consultant also works with each patient. Face transplantation provokes debate on many complex ethical issues, as I’ve learned as section editor of ethical, legal and financial considerations for Current Opinions in Organ Transplantation. For example, in 2005, the world’s first face transplant patient, in France, received lucrative film deals and other incentives that complicated her consideration of the surgery. We take great strides to assist patients in managing distinct challenges like this that can arise with face transplantation.
Advertisement
In addition, Cleveland Clinic media experts help coach candidates for the anticipated increase in media attention surrounding them and their surgery.
Connie, the recipient of the first near-total face transplant at Cleveland Clinic, wondered if her grandson and her dog would recognize her after surgery. When both visited, they knew her instantly.
Patients should be educated that identity is an internal quality — and not indicated solely by one’s face. Elements of identity are in one’s voice, gestures and physicality. Reinforcing this truth helps reassure patients before transplant and ease their transition into post-transplant life.
One of the most important factors in psychological healing after face transplant is social reintegration with family and friends. However, it does not happen easily.
Social isolation is common for patients with severe facial wounds and deformities. They often require care in skilled nursing facilities, which removes them from their established communities. Some cease all public interaction so they can avoid the stares, questions and insensitive comments from passersby.
For example, Connie had very little contact with her extended family prior to transplant. Speaking was difficult for her, and her speech was hard to understand. Communication had become a source of frustration for her and others.
Following Connie’s face transplant, her speech improved significantly. She rekindled family relationships and resumed social activities. She became a promotional speaker for organ donation and domestic violence groups. But these successes came only after extensive counseling to help her overcome past hurts, including strangers’ distressing reactions and abusive comments pre-transplant.
Advertisement
Seeing someone with a facial disfigurement can be disconcerting, even for medical professionals. I think it helps any physician, especially psychiatrists, to have experience treating patients with facial deformities (such as in a burn unit) before working with face transplant patients.
Also, it often takes a great deal of time to decipher speech patterns and understand a patient’s self-expression, particularly in those with a damaged palate or missing teeth. Patients with visual impairments may not be able to write or type either. Communication can require much repetition and patience, as well as the understanding that social interaction may be undesirable for them.
But humans are, at essence, social beings. We seek to interact with one another. Facial transplantation combined with the right psychological care can enable those with deformities to reclaim their identity, reestablish their social contacts and ultimately get their life back.
Dr. Coffman is a psychiatrist in Cleveland Clinic’s Department of Psychiatry and Psychology.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade