Additional screening, longer prophylaxis may be needed
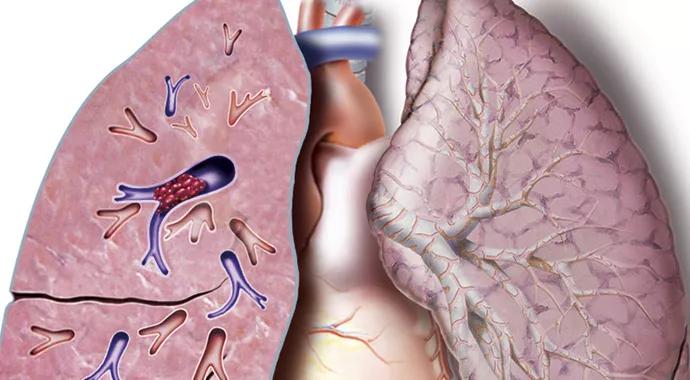
A study of Cleveland Clinic pneumonectomy patients has found that the risk of venous thromboembolism (VTE) peaks at six days after the surgery and remains elevated for up to 30 days.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The presence of VTE after pneumonectomy is higher than we previously thought, suggesting the need for additional screening or longer prophylaxis,” says Siva Raja, MD, PhD, who presented the study at the 95th Annual Meeting of the American Association for Thoracic Surgery earlier this year. “As a result, we are looking into the feasibility of increasing VTE prophylaxis in this high-risk thoracic surgery population for up to 30 days.”
The study included all 112 patients who underwent pneumonectomy at Cleveland Clinic for benign and malignant conditions from 2006 — when Cleveland Clinic adopted routine predischarge VTE screening following pneumonectomy —to 2013. All received comprehensive VTE prophylaxis (early ambulation, 5,000 units of subcutaneous unfractionated heparin twice daily and use of lower-extremity compression stockings) and underwent lower-extremity VTE screening with duplex ultrasound prior to discharge.
These patients were compared with a previously published cohort of 336 Cleveland Clinic patients who had undergone pneumonectomy without routine VTE screening prior to 2006.
Symptomatic VTE is associated with a poor prognosis. However, the prevalence, timing and clinical importance of both symptomatic and asymptomatic VTE after pneumonectomy were unclear.
Overall, 20 of the 112 patients in the screened group had VTE at some point during follow-up:
Advertisement
The researchers found that the prevalence of in-hospital VTE was nearly three times higher in the screened group than in the nonscreened group (8.9 percent vs. 3.0 percent; P = .008). Moreover, the 30-day prevalence of VTE was more than twice as high in the screened group than in their nonscreened counterparts (12.5 percent vs. 5.0 percent; P = .007).
In both cohorts, VTE occurrence peaked approximately six days after pneumonectomy (around the day of discharge) and plateaued after 30 days.
Despite standard prophylaxis, the prevalence of VTE in screened patients was higher than previously reported in unscreened patients. “The more we looked, the more we saw,” says Dr. Raja. “We found a nearly threefold increase in in-hospital prevalence when routine predischarge screening was initiated and a twofold increase in late follow-up.”
They also found that two-thirds of below-the-knee deep vein thromboses progressed, requiring therapeutic anticoagulation.
VTEs are especially problematic in patients who have undergone pneumonectomy, Dr. Raja points out, since these individuals usually have low pulmonary reserve for withstanding the effects of pulmonary embolism.
In fact, his study showed that the presence of a VTE — whether symptomatic or asymptomatic — portended worse long-term survival: Only 66 percent of patients who experienced a VTE were alive at 1 year, compared with 85 percent of patients who did not develop a VTE.
“This quality-improvement initiative revealed a substantially higher prevalence of post-pneumonectomy VTE than in our unscreened population,” notes Dr. Raja. “Despite a single screening, VTE occurred after discharge.”
Advertisement
“Based on this increased prevalence and elevated risk to at least 30 days, we changed our standard prophylaxis to 40 mg of low-molecular-weight heparin daily,” he adds.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable