INTERMACS analysis sets the stage for a confirmatory randomized trial
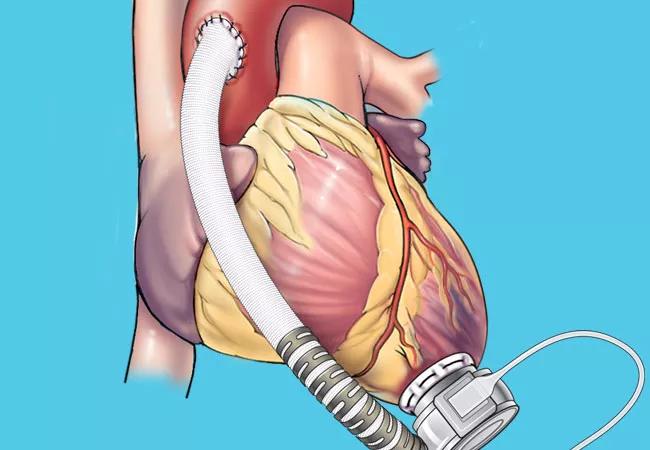
Use of phosphodiesterase 5 (PDE5) inhibitors after left ventricular assist device (LVAD) implantation is associated with a significantly lower rate of thrombotic events and with improved survival, according to an analysis of nearly 14,000 recipients of continuous-flow LVADs in the national INTERMACS registry.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This observational evidence of a reduction in thrombotic events — specifically, LVAD thrombosis and/or ischemic stroke — signals a pressing need for a randomized controlled trial to confirm the apparent benefit of postimplant use of PDE5 inhibitors for patients receiving either centrifugal or axial LVADs,” says Randall Starling, MD, MPH, senior author of the Cleveland Clinic-led analysis, which was published online in July by the Journal of the American Heart Association.
The investigation was spurred by preliminary findings from single-center analyses suggesting that sildenafil, the most commonly used PDE5 inhibitor, may be associated with a reduced incidence of LVAD pump thrombosis and ischemic stroke.
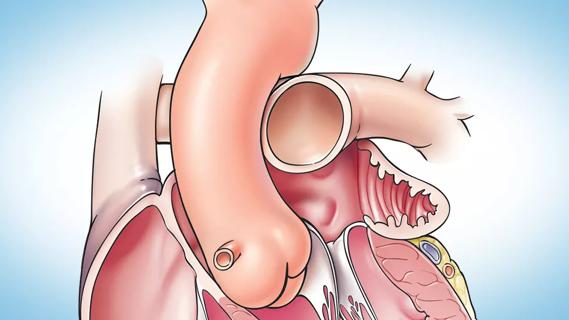
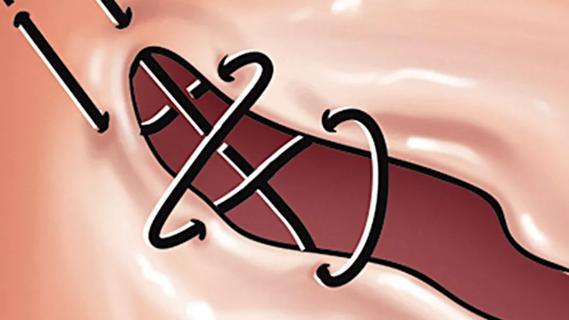
Those findings are consistent with the fact that PDE5 inhibitors enhance nitric oxide-mediated vasodilation by inhibiting cGMP degradation and demonstrate antiplatelet and antithrombotic effects. “Sildenafil is frequently used to unload the right ventricle in patients with LVADs, and some have proposed that it and other PDE5 inhibitors may influence not only hemodynamics but hemostasis as well,” says Dr. Starling, a Cleveland Clinic heart failure cardiologist. “There is interest in whether PDE5 inhibitor therapy should be added to anticoagulation and antiplatelet therapies to mitigate the risk of LVAD thrombosis.”
“Although recent improvements in LVAD design have significantly lowered the risk of pump thrombosis compared with the era of older LVAD technologies, rates of LVAD-related stroke and gastrointestinal bleeding are still high enough to demand further exploration of interventions to reduce these complications,” adds study co-author Edward Soltesz, MD, MPH, Surgical Director of Cleveland Clinic’s Kaufman Center for Heart Failure Treatment and Recovery.
Advertisement
The researchers analyzed data from all patients who underwent primary LVAD implantation in the national INTERMACS (Interagency Registry for Mechanically Assisted Circulatory Support) database from 2012 to 2017. The 13,772 eligible patients were divided into those who did (n = 4,950) or did not (n = 8,822) receive a PDE5 inhibitor after implantation. The two groups were compared in terms of incidence of pump thrombosis or ischemic stroke (composite primary endpoint) and all-cause mortality (secondary endpoint) during LVAD support over 48 months of follow-up.
Patients in the PDE5 inhibitor group had significantly lower rates of all major outcomes of interest relative to those in the no-PDE5 inhibitor group, as follows:
Notably, the results favoring post-implantation PDE5 inhibitor use were observed with both axial LVADs and newer centrifugal LVADs.
These benefits were achieved with one notable downside: the incidence of gastrointestinal bleeding was significantly higher in patients who received a PDE5 inhibitor than in those who did not (HR = 1.14; 95% CI, 1.06-1.23; P < 0.01). “This finding merits further investigation, as gastrointestinal bleeding is a major source of LVAD-associated morbidity,” says Dr. Starling.
Advertisement
The researchers point out that the reduction in thrombotic events with post-implant PDE5 inhibitor use was observed in the context of similar and conventional antithrombotic treatment regimens between the groups who did and did not receive PDE5 inhibitors.
Additionally, the authors used a robust statistical method — inverse probability of treatment weighting—to attenuate the risk of confounding from differences in comorbidities and demographic profiles between the groups. “Our findings were corroborated by three independent statisticians, including Kathy Wolski, MPH, lead biostatistician of the Cleveland Clinic Coordinating Center for Clinical Research (C5Research), and represent two years of work during my heart failure research fellowship at Cleveland Clinic,” says lead author Andrew Xanthopoulos, MD, PhD, currently at the University of Thessaly, Larissa, Greece.
“Ultimately, the results of [this] analysis expand our understanding of potential indications for PDE5 inhibitors beyond treatment of pulmonary vascular disease and right heart failure to include potential prevention of thromboembolic complications,” observes an editorial accompanying the study in the Journal of the American Heart Association.
Nevertheless, the Cleveland Clinic investigators note that their analysis was limited by its nonrandomized, observational nature and that other limitations include its inability to assess for the dosage, timing and duration of PDE5 inhibitor therapy. “These are questions that should be explored in a randomized controlled trial to definitively address whether and how PDE5 inhibitors should be added to the medical regimen of LVAD recipients,” concludes Dr. Soltesz. “We hope to help such a trial get underway before long.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
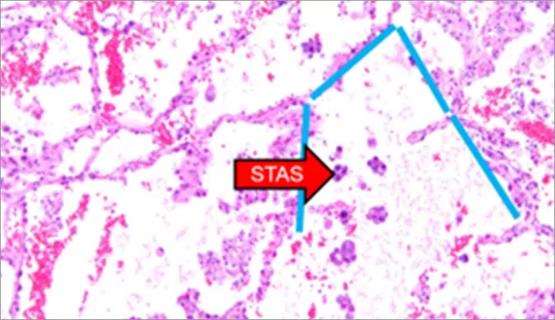
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable