Findings hint at potentially easier treatment initiation vs. other S1P receptor modulators
Once-daily oral ozanimod, a sphingosine 1-phosphate (S1P) receptor modulator, was well tolerated and resulted in significantly lower relapse rates than weekly intramuscular interferon beta-1a therapy in two large international phase 3 trials involving patients with relapsing multiple sclerosis (MS).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Results from the trials — SUNBEAM and RADIANCE — were published online Sept. 3, 2019, in The Lancet Neurology.
An approval decision is expected from the FDA by late March 2020 for use of the drug in treating relapsing forms of MS. If approved, ozanimod will join two other S1P receptor modulators — fingolimod (FDA-approved in September 2010) and siponimod (approved in March 2019) — for this indication.
“In the phase 2 and phase 3 experience we now have with ozanimod, it compared favorably with the other two available drugs in its class,” says Jeffrey A. Cohen, MD, senior author of the SUNBEAM trial and lead author of the RADIANCE trial. “If approved, ozanimod is expected to offer an important new treatment option for relapsing MS.” Dr. Cohen is Director of Experimental Therapeutics in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research.
Both trials were double-blind, double-dummy, active-control phase 3 investigations that compared ozanimod (1.0 mg or 0.5 mg daily) to interferon beta-1a (30 μg weekly). SUNBEAM enrolled 1,346 participants across 152 sites and provided at least 12 months of treatment (mean, 13.6 months). RADIANCE, with 1,320 participants at 147 sites, lasted 24 months.
Key findings from the trials included:
Advertisement
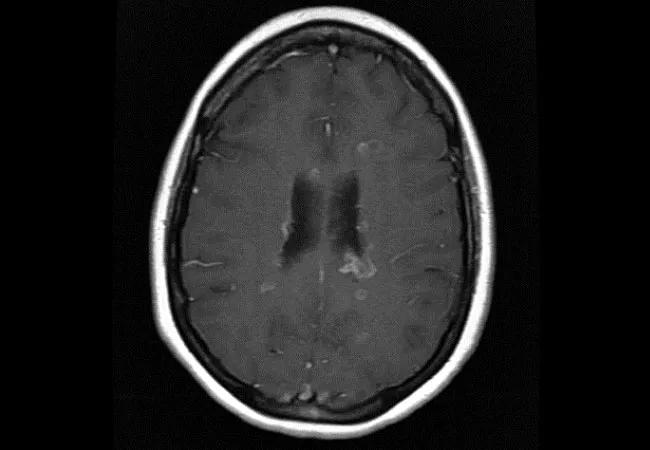
The slowing of thalamic volume loss is a particularly promising finding, according to Dr. Cohen, who believes this is the first time such a finding has been reported in phase 3 testing of an MS drug.
“Neurologists regard the thalamus as a kind of thermostat for brain damage, as so many neural pathways pass through it,” he explains. “Reduced volume loss suggests that ozanimod might offer some protection against structural harm associated with MS progression.”
Five subtypes of S1P receptors have been described. While fingolimod is nonselective, both siponimod and ozanimod interact with receptor subtypes 1 and 5 with high affinity, which is believed to account for efficacy.
“The results met our higher expectations for a selective S1P receptor modulator,” says Dr. Cohen. “Good efficacy was combined with reduction of most of the safety concerns sometimes seen with this drug class.”
Investigators particularly looked out for the following:
Advertisement
Editorialists in an accompanying Lancet Neurology commentary noted: “If ozanimod attains regulatory approval without requiring universal first-dose observation of CYP2C9 genotyping, it might improve start-up feasibility, particularly in resource-poor areas.”
Dr. Cohen says that if ozanimod is approved, it would be reasonable to use it as first-line therapy for patients recently diagnosed with relapsing MS and as an alternative for those who failed other treatments because of relapse or adverse effects.
“The availability of multiple treatment options enables us to better personalize medicine and find a drug that best suits each patient,” he adds.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade