ATTRACT trial finds no reduced risk versus anticoagulation alone following DVT
Pharmacomechanical catheter-directed thrombolysis to manage deep vein thrombosis (DVT) does not reduce the risk of post-thrombotic syndrome over anticoagulation alone, but it does increase the risk of major bleeding. So conclude researchers with the multicenter phase 3 ATTRACT trial (Acute Venous Thrombosis: Thrombus Removal with Adjunctive Catheter-Directed Thrombolysis) in a paper published Dec. 7 in The New England Journal of Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The ATTRACT trial has provided data showing that first-line therapy for most patients with DVT should remain anticoagulation without pharmacomechanical thrombolysis,” says study co-author and Cleveland Clinic vascular medicine physician Heather Gornik, MD, who served on the trial’s steering committee. Cleveland Clinic was an enrolling site for the study.
Post-thrombotic syndrome occurs in up to half of patients within two years of a DVT, causing chronic limb pain and swelling that can progress to major disability, leg ulcers and impaired quality of life. The ATTRACT researchers hypothesized that catheter delivery of a fibrinolytic drug into the thrombus along with mechanical aspiration or maceration of the thrombus — i.e., “pharmacomechanical thrombolysis” — would reduce the risk of this outcome with minimal risk of significant bleeding.
To test that hypothesis, they enrolled 692 patients with acute proximal DVT involving the femoral, common femoral or iliac veins into the 24-month ATTRACT study. Patients were randomized in an open-label, assessor-blinded manner to receive anticoagulation and compression stockings alone (control group) or anticoagulation and compression stockings plus pharmacomechanical thrombolysis (intervention group).
Approximately half of patients in both groups developed post-thrombotic syndrome between six and 24 months after treatment (48 percent of the control group and 47 percent of the intervention group). Failure of the pharmacomechanical intervention to prevent post-thrombotic syndrome could not be attributed to inadequate removal of the thrombus, as venography was performed to confirm degree of thrombus removal.
Advertisement
Pharmacomechanical thrombolysis was associated with an advantage in one secondary outcome measure — severity of post-thrombotic syndrome — as patients in the intervention group were less likely than controls to experience moderate to severe pain and swelling in the affected limb (18 percent vs. 24 percent; P = .04).
However, major bleeding events within 10 days of treatment occurred significantly more often in the intervention group than in the control group (1.7 percent vs. 0.3 percent; P = .049), although there were no fatal or intracranial bleeds.
“I was disappointed by the results because we were hoping to find a treatment that could be broadly applied to prevent post-thrombotic syndrome,” says Dr. Gornik. “Unfortunately, this was not the case.”
She and her fellow researchers were surprised that the ATTRACT findings differed from those of the recent CAVENT trial, which showed a reduction in the risk of post-thrombotic syndrome over two to five years after DVT treatment.
Dr. Gornik says the two studies’ results may have differed because CAVENT enrolled patients with more central, larger iliofemoral DVTs, whereas ATTRACT enrolled patients with both iliofemoral and femoral-popliteal DVTs. “CAVENT also used different techniques to treat the DVTs than were used in ATTRACT,” she adds. In addition, ATTRACT enrolled more than three times as many subjects as CAVENT (N = 209) and was conducted at 56 centers in the United States, whereas CAVENT patients all came from four Norwegian centers.
Advertisement
“I’m looking forward to future analyses from the ATTRACT data set, as they may provide insights into differences between findings of the two trials,” Dr. Gornik notes.
She says the takeaway message for clinicians is that anticoagulation alone is first-line therapy for DVT. “ATTRACT supports current practice that the majority of patients with DVT, and particularly those with mild or moderate symptoms, can be treated with best medical therapy and not referred to an interventionalist,” says Dr. Gornik. “This was a negative study overall, and it’s important to note that.”
She adds, however, that some of the subset data and secondary end points provide evidence that patients with more extensive DVT and more severe symptoms may have derived some benefit from pharmacomechanical thrombolysis. “Much work remains in developing new treatment strategies to prevent patients with DVT from developing post-thrombotic syndrome. I think future studies will explore identifying which high-risk patients may benefit from this intervention.”
For now, she says, pharmacomechanical thrombolysis appears most applicable for patients with severe symptoms despite medical therapy (anticoagulation and compression stockings), extensive thrombus burden and proximal vein involvement — and especially for younger patients with good functional capacity and low bleeding risk. “It also has a clear role in patients with phlegmasia cerulea dolens — an extensive, very severe form of DVT causing impaired tissue perfusion and threatening the limb. Those patients require an immediate interventional appraoch,” she observes.
Advertisement
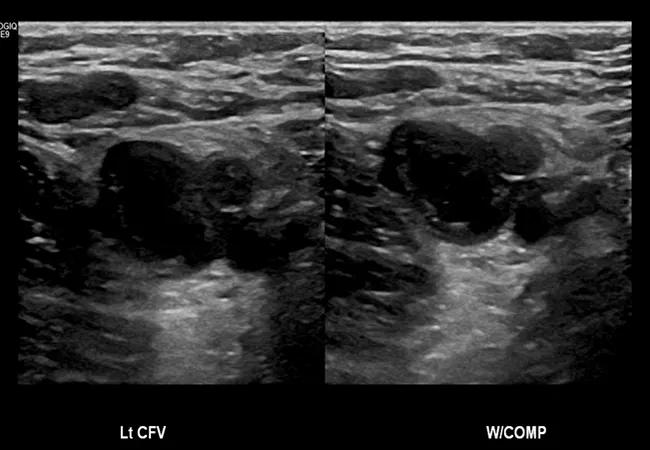
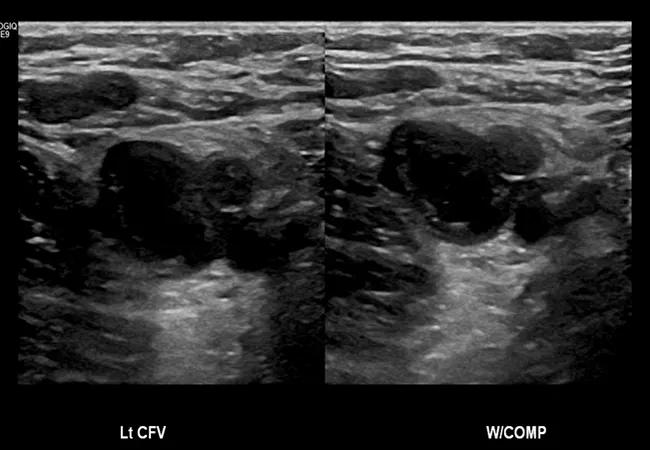
Figure. Ultrasound showing a thrombus in the left common femoral vein that is inhibiting compression of the vein.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable