Study shows that intravitreal injections may significantly slow the disease once thought untreatable
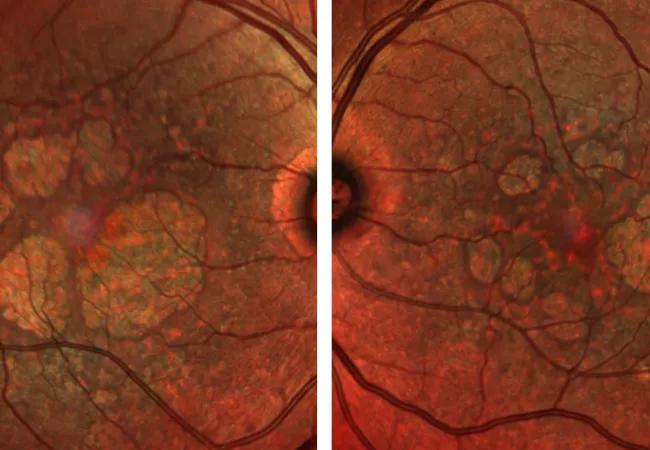
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56456daa-2178-4f59-91f7-09c858af3ea1/21-EYE-2468413-CQD-Efficiancy-and-safety-Rishi-Singh-650x450-1_jpg)
21-EYE-2468413-CQD-Efficiancy and safety Rishi Singh 650×450
There is currently no treatment for geographic atrophy — the “dry” form of macular degeneration, a leading cause of blindness in the U.S. and worldwide. Now a new study has shown that the drug pegcetacoplan can significantly slow the disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Two phase 3 clinical trials showed that injecting pegcetacoplan monthly and every other month resulted in a significant reduction in lesion growth. The study also found that pegcetacoplan was generally safe and well tolerated, although a small number of patients converted to “wet” macular degeneration, which is treatable.
“This is a first step in treating this debilitating disease,” says ophthalmologist and retina specialist Rishi P. Singh, MD, of Cleveland Clinic’s Cole Eye Institute. “It represents a breakthrough therapy for patients with this condition and potentially could reduce legal blindness around the world.”
Dr. Singh presented the top-line findings from the phase 3 study at the American Academy of Ophthalmology 2021 meeting.
The study built on previous research that showed that dry macular degeneration is linked to the complement system and a hyperactive immune response that damages the eyes. Pegcetacoplan is a complement system inhibitor that has previously been used to treat paroxysmal nocturnal hemoglobinuria, a rare autoimmune disorder linked to a systemic complement cascade.
The study involved two multicenter, phase 3 clinical trials (DERBY and OAKS) involving a total of more than 1,250 patients with geographic atrophy. Patients were randomized to receive injections of 15 mg of pegcetacoplan monthly or every other month, or a sham injection monthly or every other month.
In the combined results of the two trials, patients who received the drug monthly showed a 17% reduction in geographic atrophy lesions after 12 months, compared to those who received sham injections, while those who were injected every other month had a 14% reduction.
Advertisement
Patients with extrafoveal lesions had an even stronger response, with a 26% reduction in lesions with monthly injections and 23% reduction with every-other-month injections compared to the sham group.
“We expected this drug to work, but it exceeded my expectations,” says Dr. Singh.
The drug was generally safe and well-tolerated. The most common side effects were conjunctival hemorrhage, eye pain and vitreous floaters.
However, around 7% of patients developed wet macular degeneration as a result of the medication, not as a normal progression of the disease.
“That’s definitely a concern,” says Dr. Singh. “While this is breakthrough therapy, the conversions to wet macular degeneration are noteworthy for clinicians and patients.”
Wet macular degeneration can be treated with currently available anti-VEGF agents, he notes.
Results of the study are planned to be submitted to the FDA for review by the end of 2021, with a decision on FDA approval for clinical use anticipated in early 2022.
Dr. Singh said the findings are a significant step forward in the treatment of macular degeneration, which affects an estimated 1 million people in the U.S.
“For years we’ve been telling ophthalmologists and patients that there’s no treatment for this condition — that it’s just a matter of aging, that its progression is inevitable over time and that there’s nothing we can do,” he says. “Finally, this drug can show a reduced progression of the disease if given monthly or every other month. It’s a game changer.”
Advertisement
Advertisement
Advertisement
Early data shows risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis
Identifies weak spots in the cornea before shape change occurs
Study highlights the value of quantitative ultra-widefield angiography
Switching medications may decrease treatment burden and macular fluid
Interventions abound for active and stable phases of TED
Corneal imaging and interpretation play a major role
Cole Eye Institute imaging specialists are equal parts technician, artist and diagnostician
Effect of low-dose atropine and dual-focus contact lenses is unknown in patients with comorbid eye conditions