Enhanced protocols and more research warranted
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
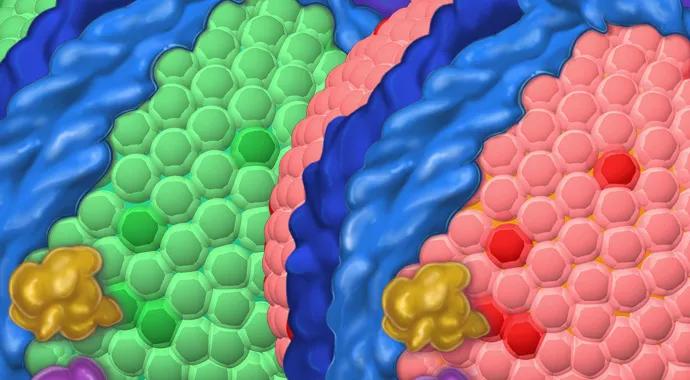
Patients with psoriatic arthritis (PsA) are at increased risk for cardiovascular disease (CVD), yet consensus guidelines for treating these patients are not available in the United States. As a result, the appropriate steps for assessing and modifying CVD risk in PsA have not been identified and disseminated.
Patients with PsA suffer from more severe atherosclerosis than patients with psoriasis alone. Studies have shown that subclinical atherosclerosis in PsA is prevalent, even in the absence of traditional CVD risk factors, suggesting a role for systemic inflammation.
The presence of carotid plaque may be used as a surrogate for CVD. Rates of carotid plaque are high in PsA, and these patients should be considered at very high risk of CVD. We conducted a study to determine whether referring PsA patients with known carotid plaque to the Heart and Vascular Institute’s Preventive Cardiology Program would result in steps to lower CVD risk.
Eighty-seven patients with PsA who presented to Cleveland Clinic rheumatologists for evaluation enrolled in our Cardiometabolic Outcome Measures in Psoriatric Arthritis Study (COMPASS) and were screened for carotid plaque using carotid duplex ultrasound. Carotid plaque was identified in 34 of 87 patients (39 percent).
Cardiac risk factors were prevalent in this cohort: 8 percent had a history of CVD, 18 percent had diabetes, 46 percent had hypertension and 49 percent had a history of smoking (Table). Only four patients with plaque had been diagnosed with CVD, and only two of these were on maximum-dose statin therapy. Factors that correlated with the presence of carotid plaque included age over 50 and elevated triglyceride levels, and patients who trended toward higher levels of smoking, diabetes and elevated LDL cholesterol levels.
Advertisement
All 87 patients were automatically referred to Cleveland Clinic’s Preventive Cardiology Program through the EPIC electronic best practice alert system. The program provides nutritional counseling, exercise instruction, lifestyle and behavioral counseling, smoking cessation programs, medical management of CVD risk factors, psychological counseling and referral to other medical specialists as needed. It also offers a program designed for patients with inflammatory arthritides that includes lifestyle counseling, an LDL goal of < 100 mg/d, cholesterol-lowering medications, and antiplatelet medications for patients as indicated.
Despite their elevated cardiac risk, only nine of the 87 patients in our cohort completed their preventive cardiology appointment.
Even when multiple strategies were available to address CVD risk in patients with PsA, few took advantage of the opportunity. Incorporation of automatic referrals to a preventive cardiology program in the same institution were not widely implemented for reasons that are unclear. It may have been perceived as too time consuming or of too little value to patients.
Although small sample size and short follow-up may have limited our study results, it appears that lack of appreciation of CVD risk by patients, primary providers and specialists may be responsible for the low rate of implementation for preventive CVD care. Early establishment of the level of CVD risk has the potential to improve CVD outcomes, but an effective screening method remains unclear for patients with elevated baseline risk. We feel that enhanced protocols for CVD risk assessment as well as more comprehensive research regarding CVD in PsA are urgently needed.
Advertisement
Dr. Husni (husnie@ccf.org; 216.445.1853) directs both the Arthritis and Musculoskeletal Treatment Center and Cleveland Clinic’s Psoriatic Disease Biorepository.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable