Study shows no effect on complications
By Toru Sugihara, MD, MPH, and Michael Kattan, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Mechanical bowel preparation (MBP) is the mechanical removal of feces from the intestines. Preoperative MBP is considered standard care for surgery involving the abdomen or pelvic area. This procedure has been widely accepted among surgeons since its introduction by Sir William Halsted in the late 19th century. Dogmatically, it is believed that MBP is beneficial for reducing the volume of bowel contents and the total amount of bacteria in the colon.
Though a recent Cochrane Review summarized that MBP is not an efficient procedure in open colon surgery, studies evaluating the benefit of MBP in laparoscopic surgery are limited. Many laparoscopic surgeons opt for MBP preoperatively because they believe that MBP can decompress the bowel and make more room for surgery in the intra-abdominal space.
On the other hand, it is recognized that MBP may have multiple adverse side effects, including causing discomfort, insomnia, weakness, abdominal distension and an electrolyte disturbance, especially in dehydrated or elderly patients. Overall, these adverse events may serve to discourage preoperative MBP in some groups of patients.
To challenge the belief that MBP improves the efficiency of the laparoscopic surgery, we performed a retrospective multicenter study and compared laparoscopic surgeries with and without MBP in both prostatectomy and nephrectomy. In the study, we employed the Japanese Diagnosis Procedure Combination database, which is highly representative of that country, and detailed information on oncological staging and medications used for MBP.
Advertisement
The definition of MBP in the study was a preoperative medication including at least one of the following drugs, all of which were approved for preoperative MBP in Japan: polyethylene glycol electrolyte solution, magnesium citrate solution and sodium picosulfate. Because of the limitation of the database and a difference in clinical customs between Japan and the United States, evaluation of fast-track diet was not included in this study.
We found 154 non-MBP cases and 580 MBP cases in prostatectomy and 1,110 non-MBP cases and 1,630 MBP cases in nephrectomy. After making a background adjustment by using age, sex, oncological staging, preoperative pre-existing comorbidities and several institutional variables, we found no significant differences between non-MBP and MBP groups in terms of overall complications, operation time and postoperative length of stay. (Table 1)

Table 1. Comparisons of outcomes between laparoscopic surgeries with and without mechanical bowel preparation
This is the first study to analyze the effect of MBP in laparoscopic urological surgeries for a large number of patients. The data suggest that MBP could be safely omitted before these surgeries. Interestingly, in reviewing the background, we collaterally learned that MBP was more often used for patients with a higher comorbidity index and at academic and high-volume hospitals. In addition, MBP was used in about 75 percent of prostatectomy cases and 60 percent of nephrectomy cases. This corroborates the prevalence of MBP in our specialty.
Advertisement
It is beyond dispute that MBP is an uncomfortable experience for patients. In addition, studies have shown that a majority of patients who received MBP reported a negative attitude toward their hospital stay and did not want to have MBP again. We hope that the evidence our study offers will help physicians foster an improvement in quality of care of patients and reduce patients’ pain during hospitalization.
At the time this article was written, Dr. Sugihara was a postdoctoral fellow in Cleveland Clinic’s Department of Quantitative Health Sciences
Dr. Kattan is Chairman of the Department of Quantitative Health Sciences.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
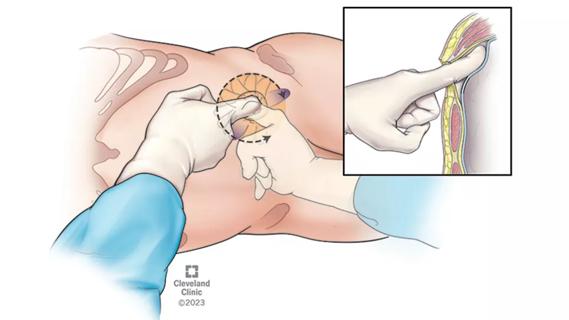
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
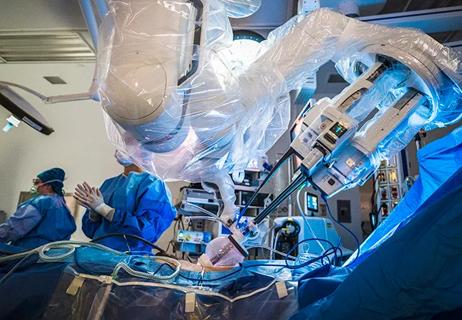
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients