Retrospective clinic-based study provides intriguing initial comparisons
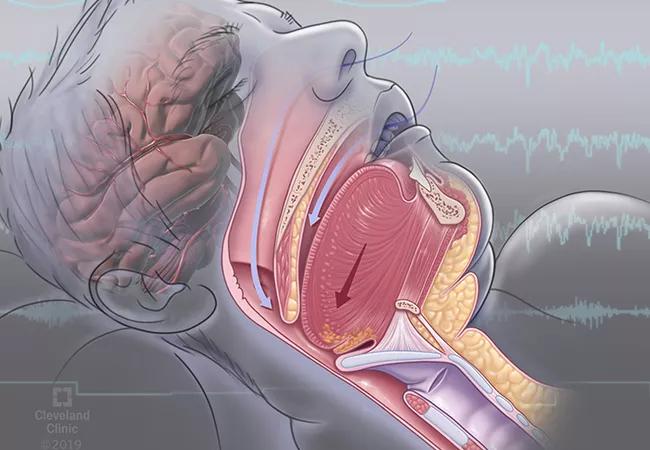
In one of the first comparative studies of the two leading interventions for obstructive sleep apnea (OSA), positive airway pressure (PAP) therapy showed an advantage in blood pressure benefit while upper airway stimulation (UAS) therapy demonstrated greater improvement in daytime sleepiness. The retrospective clinic-based cohort study was recently published online in Chest by a team of Cleveland Clinic researchers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We found interesting differences between the major therapies for OSA in clinic-based cohorts,” says principal investigator Harneet Walia, MD, of Cleveland Clinic’s Sleep Disorders Center. “These findings can help sleep clinicians provide more-informed guidance to patients who are weighing their therapy options.”
PAP, the mainstay of OSA treatment, has well-established benefits for improving daytime sleepiness. Evidence also indicates that it improves blood pressure.
UAS, which was FDA-approved in 2014 for moderate to severe OSA in patients who have not had success with PAP therapy, has been less well studied. Prior to the current analysis, no large clinic-based investigations had been published on either the impact of UAS on blood pressure or the comparative effects of PAP and UAS on blood pressure and daytime sleepiness.
For their study, Dr. Walia and colleagues drew from two different but well-matched cohorts to yield adequate numbers of UAS subjects:
All patients in both groups had to be UAS-eligible (i.e., body mass index < 35 kg/m2) and had follow-up data from two and six months after UAS implantation or PAP initiation.
After rigorous propensity matching, mixed-effect models were used to compare outcomes in 201 patients from each arm.
Advertisement
Sleepiness was assessed using the Epworth Sleepiness Scale (ESS), where higher scores reflect greater daytime sleepiness. Blood pressure was measured per standard of care at the sites where patients received care. In the Cleveland Clinic cohort, an automatic cuff was used; clinics in the ADHERE registry used either manual or automated methods.
Analysis revealed the following main findings:
Improvement in daytime sleepiness was greater with UAS. In the UAS arm, mean ESS score improved from 10.7 before treatment to 7.2 at follow-up (P < 0.001). The PAP group improved from 10.4 to 7.7 (P < 0.001). The difference in mean change between the two groups was –0.8 in favor of UAS (P = 0.046).
Improvement in blood pressure was greater with PAP. Overall, patients in the UAS arm did not have significant changes from baseline in systolic, diastolic or mean arterial pressure at approximately four-month follow-up, as follows:
However, in a subset of UAS patients with elevated baseline blood pressure, significant improvements were found at follow-up in systolic pressure (from 134.7 to 130.5 mmHg; P = 0.006) and mean arterial pressure (from 99.2 to 97.1 mmHg; P = 0.020).
In contrast, at four months the PAP arm showed statistically significant improvements in diastolic pressure (from 77.0 to 74.6 mmHg; P < 0.001) and mean arterial pressure (from 94.7 to 92.5 mmHg; P = 0.002), whereas improvement in systolic pressure reached statistical significance only in the subset of patients with elevated baseline pressures (from 139.9 to 133.7 mmHg; P < 0.001).
Advertisement
This collectively translated to significant between-group differences in mean change in diastolic pressure (–3.7 mmHg; P < 0.001) and mean arterial pressure (–2.8 mmHg; P = 0.008), both in favor of PAP.
“This study adds some intriguing insights to the literature on OSA interventions,” says Dr. Walia.
She notes that although mean weekly duration of therapy use was 6.2 hours longer with UAS than with PAP (45.4 vs. 39.2 hours/week), UAS therapy’s significant advantage in ESS benefits remained after adjustment for device adherence. “This suggests there may not be a simple dose-response relationship between the two therapies but that they may exert their effects via different mechanisms,” she explains.
She also points out potential confounders related to blood pressure findings. Because patients qualify for UAS only after having first tried PAP, it is possible that the UAS group had longer periods of OSA-related vascular dysfunction, making it less reversible. Additionally, blood pressure measurements were not conducted in a standardized fashion as they would be in a prospective clinical trial, possibly obscuring effects.
“This study was not designed to provide definitive understanding of physiologic effects, but it has generated important hypotheses for future research,” she notes.
“These findings suggest differential OSA therapy-specific cardiovascular influences,” adds senior author Reena Mehra, MD, MS, Director of Sleep Disorders Research at Cleveland Clinic. “However, future studies should be designed to better elucidate the physiologic mechanisms that underlie these observed differences.”
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade