More accurate than existing noninvasive tests
A team of Cleveland Clinic researchers developed a novel machine learning model that correctly identifies the majority of non-alcoholic fatty liver disease (NAFLD) patients with advanced fibrosis who are indeterminate by the Fibrosis-4 (FIB-4) Index.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
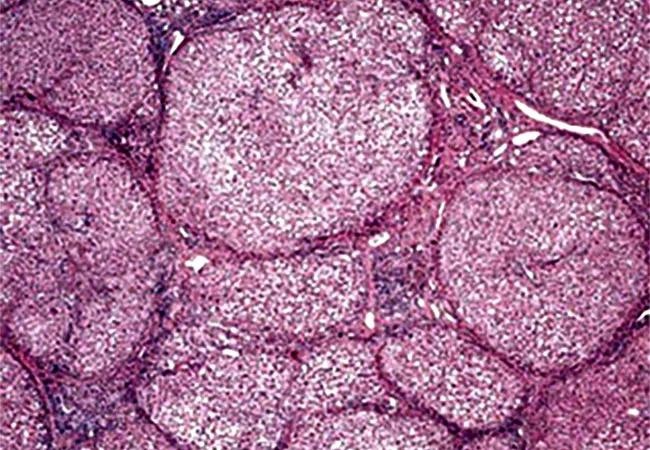
Advanced fibrosis in NAFLD is the most important predictor of mortality and liver-related morbidity. Of the noninvasive tests developed to detect fibrosis, FIB-4 is a commonly used index. However, a significant number of patients are classified as indeterminate and will require further testing and/or liver biopsy.
“Identification of liver fibrosis is crucial to guide patient management in NAFLD, which affects 30% of the world population,” explains study author Manik Aggarwal, MD, an internal medicine resident at Cleveland Clinic. “FIB-4 is a commonly used index to identify fibrosis; however, when using FIB-4, almost 40% of patients fall into the indeterminate category and require further testing, thus increasing cost and risk of morbidity and mortality.
“Machine learning has emerged as a novel tool for predictive modelling since it is able to identify complex relationships between parameters,” he continues. “So, we designed a study to see if a machine learning model can identify patients with advanced liver fibrosis who were indeterminate by the FIB-4 index.”
The study included 960 histologically confirmed NAFLD patients at Cleveland Clinic with a mean age of 50.7 years and BMI of 40.8 Kg/m2. The researchers used the NASH Clinical Research Network (NASH-CRN) criteria to score all biopsies, and advanced fibrosis was defined as fibrosis stage ≥ 3.
Thirty-six covariates were considered when building the machine learning model, including demographic, clinical and commonly measured laboratory parameters within three months of liver biopsy. The researchers built the model by segregating 20% of data into a blinded validation cohort and using the remaining 80% of data to iteratively train and test. The final model incorporated 13 features to guide the prediction of advanced fibrosis.
Advertisement
The train-test cohort (N = 768) had an area under the curve (AUC) of 0.83, and the validation cohort (N = 192) had an AUC of 0.80, according to the study authors, who report that these three cohorts had sensitivity/specificity for diagnosing advanced fibrosis of 0.86/0.67, 0.84/0.59 and 0.84/0.64.
“The machine learning model was superior to FIB-4 in diagnosing advanced fibrosis. In the validation set, the model correctly classified 71% of patients as either having or not having advanced fibrosis whereas FIB-4 index correctly identified 60% of cases,” says Dr. Aggarwal. “Thirty percent of patients were indeterminate when using FIB-4 index in the validation set. The model was able to correctly identify 80% of cases with advanced fibrosis in this subgroup, which would otherwise have required a liver biopsy.”
This machine learning model is a novel solution to the current problem with noninvasive tests and reduces the need for additional evaluation. This model, which uses covariates available at all clinical centers, has wide applicability. The study authors note that prospective studies are needed with larger cohorts to assess validity.
“Our machine learning model can be easily implemented in the electronic medical record and identify patients with advanced liver biopsy using routinely recorded clinical and lab parameters,” emphasizes Arthur McCullough, MD, staff in the Department of Gastroenterology, Hepatology & Nutrition at Cleveland Clinic.
“It can prevent liver biopsies in up to 80% of cases that were originally indeterminate by FIB-4,” he concludes. “As NAFLD affects 30% of the population, avoiding the need for costlier and more invasive tests can decrease cost, improve patient safety and help focus our attention to those patients that require closer monitoring and care.”
Advertisement
Advertisement

Strong patient communication can help clinicians choose the best treatment option

ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance

The importance of raising awareness and taking steps to mitigate these occurrences

New research indicates feasibility and helps identify which patients could benefit

Treating a patient after a complicated hernia repair led to surgical complications and chronic pain

Standardized and collaborative care improves liver transplantations

Fewer incisions and more control for surgeons

Caregiver collaboration and patient education remain critical