Infrequent injury poses surgical challenge

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4c05baf5-9286-42f5-a033-e4f03de90ec6/16-ORT-1507-Berkowitz-Hero-Image-650x450pxl_jpg)
16-ORT-1507-Berkowitz-Hero-Image-650x450pxl
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Insertional ruptures off the calcaneus account for only about 10 percent of all Achilles tendon ruptures. These less common ruptures can pose a significant surgical challenge due primarily to the frequent presence of a gap at the repair site.
For the last two years, Cleveland Clinic Department of Orthopaedic Surgery has been performing successful reconstructions using free autologous hamstring grafts for insertional gaps greater than 5 cm width.
Insertional Achilles tendon ruptures differ in several important ways from the more common midsubstance injury. Most midsubstance Achilles ruptures occur in individuals with no pre-injury symptoms and relatively normal tendons, when a supranormal stress applied to the foot exceeds the tendon’s tensile strength. Because the tendon generally lacks advanced tendinopathy, it is relatively uncommon to encounter a significant gap at the site of the rupture.
Insertional ruptures, however, often occur in people with pre-existing, symptomatic Achilles tendinopathy. Many patients have previously been evaluated for complaints of posterior heel pain, and pre-injury radiographs commonly show significant enthesophyte formation at the insertion. Moreover, the pathophysiology involves not only the tendon but also the retrocalcaneal bursa and the Haglund’s deformity of the calcaneus. Once the enthesophytes and Haglund’s deformity have been resected and the abnormal tendon debrided, a gap of 3 to 8 cm is common depending on the severity of tendinopathy. Techniques such as V-Y gastrocsoleus lengthening or gastrocnemius fascial turndown are generally adequate for gaps less than 5 cm.
Advertisement
For gaps larger than 5 cm, the standard techniques are often inadequate, but free autologous hamstring grafts offer opportunity for a stable repair.
If preoperative imaging indicates a gap greater than 5 cm, then it is easiest to begin the procedure with the patient supine, and harvest the semitendinosus and gracilis tendons as one would for anterior cruciate ligament (ACL) reconstruction. Although this adds time to the surgical procedure, it ensures the procurement of quality tendon grafts. Harvesting hamstring tendons from a prone patient is possible but technically difficult. Use of allograft tendon avoids the need for harvest altogether but must be weighed against the risk of placing a large amount of foreign material in an area with a tenuous soft-tissue envelope.
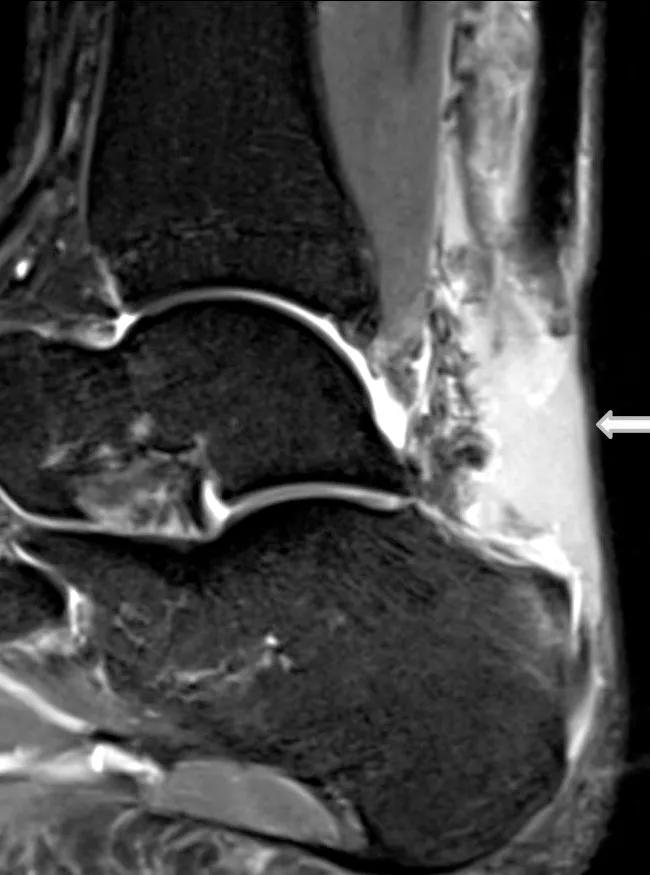
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4cb3cd25-08ff-49be-831b-a21a7dfe8027/16-ORT-1507-Berkowitz-Inset-Fig-1_jpg)
FIGURE 1 Pulvertaft weave instrument is used to pass the hamstring tendon into the Achilles.
Once the autologous hamstrings are harvested and prepared, the patient is again placed in the prone position. Surgical repair begins in standard fashion with a midline incision along the back of the leg. All thickened and fibrotic tendon is debrided, enthesophytes are sharply excised, and the Haglund’s deformity is resected with a sagittal saw.
Then the semitendinosus is weaved into the proximal limb of the ruptured Achilles using a Pulvertaft instrument. Several passes of the tendon at 90 degree angles to each other, in addition to interrupted suture, make for an extremely stable method for proximally anchoring the tendon. The tendon should be passed such that two equal limbs of semitendinosus extend out from the ruptured end of the Achilles.
Advertisement
These two limbs are then incorporated into a single Krackow suture. The tendon diameter is generally 7 to 8 mm at this time. If it is smaller, the gracilis can be added using the same technique to create a stouter distal tendon graft.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a395af8a-e53f-4252-a2d1-c1af909ea5ec/16-ORT-1507-Berkowitz-Inset-Fig-2_jpg)
FIGURE 2 The hamstring graft has been woven through the Achilles. The two limbs are then incorporated into one tendon using a Krackow suture.
Once the tendon graft is sized, it is pulled into the bone tunnel, tensioned and stabilized using the same interference screw technique utilized for short flexor hallucis longus (FHL) harvest, which is performed concomitantly. (Figures 3 and 4) The bone tunnel for the hamstring graft should be placed at least 10 mm posterior to the FHL tunnel to prevent fracture of the bone bridge.
| FIGURE 3 The hamstring graft is passed into the bone tunnel in the calcaneus. | FIG. 4 The graft is secured with an interference screw. |
|---|---|
| FIGURE 3 The hamstring graft is passed into the bone tunnel in the calcaneus. |
The patient is initially splinted in resting equinus to facilitate incision healing. After three weeks of cast/splint immobilization, the patient transitions to an orthopaedic boot with a one- to two-inch heel lift and can begin active range of motion exercises. Weight-bearing and strengthening exercises are begun at six weeks. The boot is weaned beginning at 10 to 12 weeks, and formal physical therapy proceeds from there.
Unlike the more common midsubstance injury, a gap at the injury site of insertional Achilles ruptures frequently makes successful reconstruction a challenge. For gaps greater than 5 cm, autologous hamstring reconstruction is a straightforward, reliable procedure which allows the surgeon to achieve a stable repair and ensure the best outcome for the patient.
Advertisement
Dr. Berkowitz is a staff orthopaedic surgeon who specializes in foot and ankle and lower extremity trauma surgery.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions