Study heralds potential new approach to cardiometabolic diseases
The once-improbable story linking gut microbes, TMAO and heart disease continues to build — and now the plot is beginning to turn to treatment interventions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Researchers in the Cleveland Clinic lab of Stanley Hazen, MD, PhD, have just published an animal study in Cell that demonstrates, for the first time, the potential of targeting a gut microbial pathway to treat or prevent diet-induced heart disease.
“Our findings show that we can drug the microbiome and treat a complex metabolic disease like atherosclerosis,” says Dr. Hazen, Chair of the Department of Cellular and Molecular Medicine and Section Head of Preventive Cardiology and Rehabilitation at Cleveland Clinic. “This is a proof of concept that pharmacologically manipulating the gut microbial pathway will alter susceptibility for atherosclerosis development.”
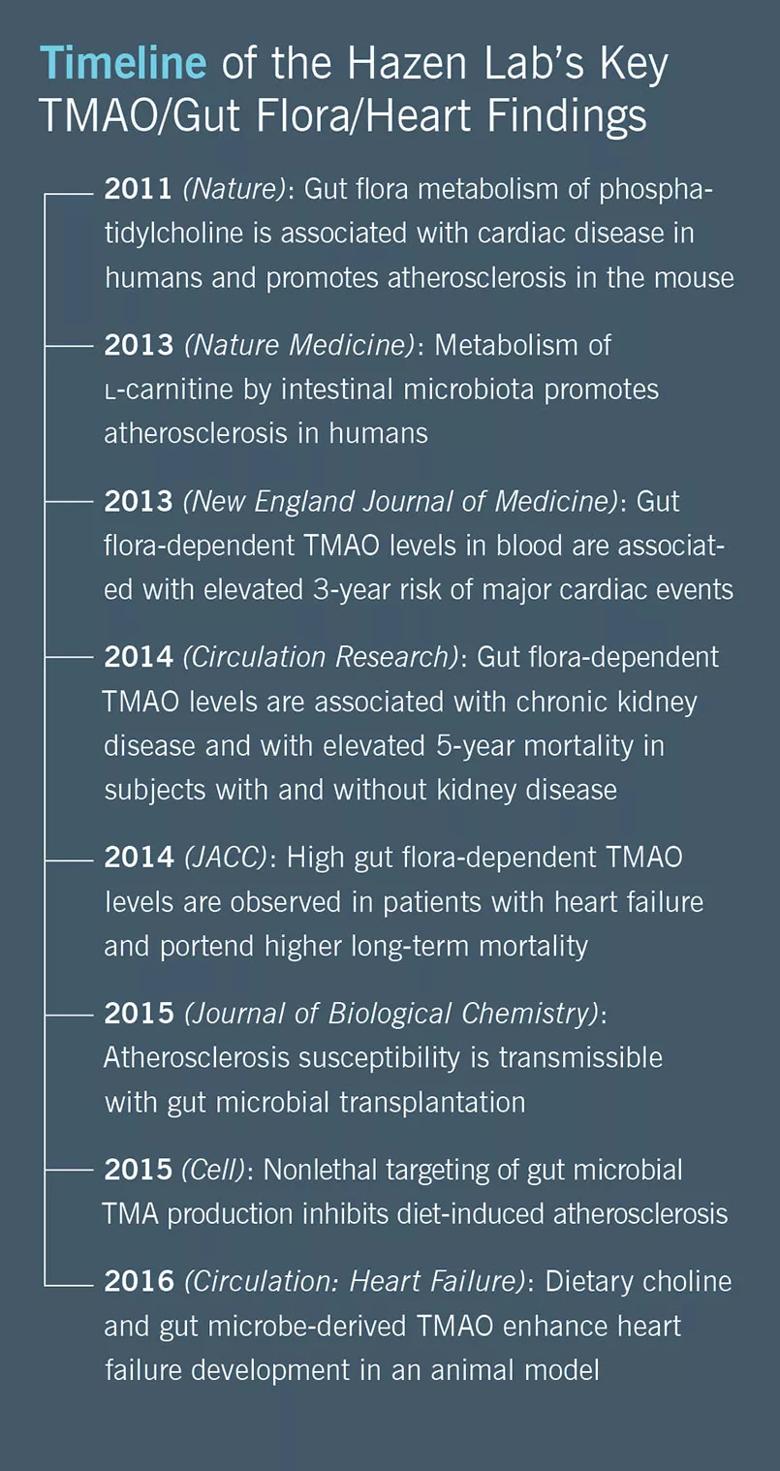
The new paper also further confirms the link between the metabolite TMAO (trimethylamine-N-oxide), gut microbes and heart disease, which Dr. Hazen’s lab first discovered more than four years ago. His research team has since extended the link to other cardiometabolic conditions such as heart failure and chronic kidney disease, as detailed in an earlier Consult QD post.
Central to this link are the nutrients choline, lecithin and carnitine, which are abundant in animal products. When these nutrients come in contact with microbes in the gut, they are metabolized into trimethylamine (TMA), which is transported to the liver and converted to TMAO. Blood levels of TMAO are associated with elevated three-year risk of myocardial infarction, stroke and death, as demonstrated by Dr. Hazen’s research team in a 4,000-patient study published in the New England Journal of Medicine in 2013.
Advertisement
The team’s new study suggests that targeted inhibition of the first step in TMAO generation — commensal microbial TMA production — can help prevent diet-induced atherosclerosis.
The researchers inhibited TMA production using the naturally occurring substance 3,3-dimethyl-1-butanol (DMB) in mice that were fed a high-choline or high-carnitine diet; control mice received the same diet without DMB supplementation. The mice that received the TMA inhibitor were found to have lower TMAO levels and to develop less atherosclerosis compared with controls. Specifically, DMB inhibited choline-enhanced endogenous macrophage foam cell formation and atherosclerotic lesion development without changes in circulating cholesterol levels.
“We were able to show that drugging the microbiome is an effective way to block this type of diet-induced heart disease,” Dr. Hazen observes.
He notes that the study exploited a metaorganismal pathway — i.e., one involving interplay between the microbes and the host. “We and others have already published findings showing that you can block diet-induced atherosclerosis at the host level by genetically knocking down flavin-containing monooxygenase 3 (FMO3),” Dr. Hazen says, “but that results in the well-documented adverse effect of the animals smelling like rotting fish.” Targeting that enzyme in humans, he explains, would likely result in something analogous to fish malodor syndrome, in which a genetic deficiency in FMO3 causes affected individuals to smell like rotting fish. That’s clearly not an acceptable side effect for what’s being pursued as a long-term therapy.
Advertisement
“There’s growing appreciation that rather than targeting the host side of the metaorganismal pathway, inhibition of microbial formation of TMA (and thus of TMAO) is of considerable interest,” Dr. Hazen says. “What’s new is that this is the first time where the target is not a Homo sapiens enzyme but a microbe enzyme. But this is otherwise much like how we use statins to inhibit cholesterol synthesis in Homo sapiens cells.”
He explains that DMB was chosen as the TMA inhibitor for the study because it’s a naturally occurring product found in some cold-pressed extra virgin olive oils and in grape seed oils. “It’s a very low-toxicity inhibitor,” he notes, “so you can give it at high levels and still observe a very mild side effect profile, as we did in this study. DMB is metabolized by the same enzyme that ethanol is, and it’s virtually completely metabolized by the liver. As a result, you’re not getting any systemic exposure to it, which is what you want when targeting a site like the gut.”
Another key distinction is that DMB is a nonlethal inhibitor rather than an antimicrobial. “The efficacy demonstrated with this nonlethal approach suggests we can target a specific microbial pathway while protecting the gut flora and avoiding antibiotic overuse and resistance, which is of course a growing problem,” Dr. Hazen says.
Despite these merits of DMB, Dr. Hazen notes that his team is also exploring the use of other, more-potent inhibitors of TMA/TMAO.
And they are actively exploring opportunities to take this approach of nonlethal gut microbial TMAO inhibition into human studies of cardiometabolic diseases, though Dr. Hazen is quick to note that clinical outcome studies will take considerable time and funding.
Advertisement
“My hope is that down the road, this type of pharmacologic approach to lowering TMAO can be used to augment statin therapy and other approaches for reducing risk in people at elevated risk of cardiovascular events,” he says. “The intervention trials remain to be done and we still have a long way to go, but I think the story is growing.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable