28-patient series suggests other dosages, delivery approaches should be studied
In the largest reported cohort to be treated with intraventricular milrinone and intravenous (IV) milrinone for cerebral vasospasm (CVS) following an aneurysmal subarachnoid hemorrhage (aSAH), no benefit was found by transcranial Doppler ultrasonography or clinical measures. So reported Cleveland Clinic researchers in a February 20 poster presentation at the 2020 International Stroke Conference.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Neither intraventricular milrinone alone nor intraventricular milrinone coupled with intravenous milrinone was beneficial for treating vasospasm in our patients with aneurysmal subarachnoid hemorrhage,” says Cleveland Clinic neurologist Pravin George, DO, the study’s primary investigator. “But with a dearth of effective therapies for this devastating condition, it is worthwhile continuing to pursue milrinone treatment, considering the suggestions of effectiveness in other studies.”
Milrinone, an inotropic and vasodilatory agent, is one of several medications and other measures that have been tried to treat CVS, a cause of delayed strokes that commonly occurs from days to weeks following apparent recovery from aSAH. It results in death or severe deficits in about 20% of cases.
Several case reports of milrinone therapy in this setting have suggested some benefit, as has as a series of 99 patients from Japan (J Neurosurg. 2018;128:717-722) treated with intrathecal milrinone injection (provided in eight-hour cycles for 14 days), which found significantly fewer delayed cerebral ischemia events compared with matched controls. An earlier case study from Cleveland Clinic (Cureus. 2018 Jul 3;10:e2916) demonstrated improvement of vasospasm following IV milrinone despite the patient having normal cardiac function, suggesting that the drug may have benefits beyond augmenting cardiac output.
The current study was a retrospective analysis of 28 consecutive patients (75% female, 75% white) with aSAH treated with intraventricular milrinone at Cleveland Clinic between January 2016 and December 2018. Patients received this treatment if they had symptomatic CVS or transcranial Doppler findings suggestive of critical CVS that persisted despite blood pressure augmentation or endovascular therapies. Patients received from 1 to 30 doses (median, 10.5; interquartile range, 6-21) of intraventricular milrinone (0.87 mg every 6 to 8 hours) over a period of up to 21 days.
Advertisement
Of this cohort, 21 patients (75%) were also treated with IV milrinone, dosed in a standard fashion based on the Montreal Neurological Institute protocol. All patients also received enteral nimodipine as standard of care.
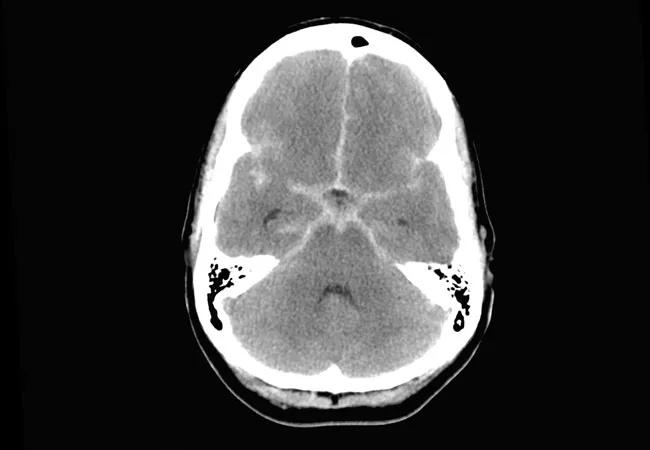
On the modified Fisher scale, 64% of patients had grade 4 SAH (thick with intraventricular hemorrhage) and 28% had grade 3 SAH (thick without intraventricular hemorrhage). Grades on the Hunt and Hess scale, where higher grades indicate greater SAH severity, broke down as follows: 32% had grades 1 or 2, 24% had grade 3, and 44% had grades 4 or 5.
No significant post-therapeutic improvement was found in transcranial Doppler velocities or CVS symptoms, regardless of whether patients were treated with intraventricular milrinone alone (P = 0.611) or intraventricular plus IV milrinone (P = 0.69). Likewise, no association was detected between improvement and timing or number of intraventricular milrinone doses.
Although no direct complications arose from milrinone therapy, the number of intraventricular doses correlated with increased (worse) modified Rankin score at discharge (P = 0.05).
Dr. George asserts that despite the lack of benefit in this study, milrinone may yet turn out to be an important therapy, as it has sound theoretical benefits and intriguing suggestions of efficacy from the literature. He notes that although Cleveland Clinic tried to develop an intraventricular dosing strategy that mimicked the intrathecal strategy used in the Japanese study, it was not the same. In addition, the wide variation in the number of intraventricular milrinone doses among patients in the Cleveland Clinic experience limited comparability.
Advertisement
Based on observations from this Cleveland Clinic experience, Dr. George would like to see more research — ideally a randomized trial with standardized protocols — with the following changes to the approach used in this series:
“There are still many unknowns about what might be an effective application of milrinone in this setting,” Dr. George says. “Without good alternatives, I don’t think we should give up on this direction yet.”
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade