Multimodal approach enables early mobilization, discharge

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Spine fusion for progressive deformity due to idiopathic scoliosis remains the gold standard for definitive treatment. It is a reliable technique for preventing progression as well as the long-term cardiopulmonary sequelae that progressive curves produce when severe.
Unfortunately, fusion is historically accompanied by significant perioperative morbidity and prolonged hospital stays for these largely healthy patients. Hospital stays averaging nearly seven days are common in some centers and required for adequate pain control and mobilization.
Recent radical changes in postoperative pain management protocols for these cases at Cleveland Clinic have resulted in a significant reduction in perioperative morbidity, pain and ultimate length of stay for patients undergoing spine fusion for deformity. A more aggressive approach to pain management and mobilization cut our average length of stay nearly in half.
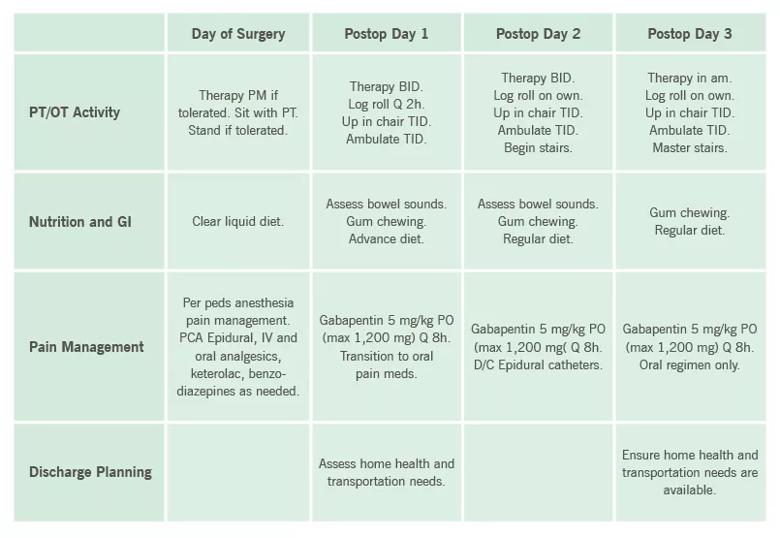
Our new protocol, patterned after a successful pilot at Children’s Healthcare of Atlanta, employs a multimodal approach to aggressive pain management and mobilization with physical therapy during the patient’s hospital stay:
These modalities have excellent perioperative analgesic properties, which allow early mobilization and, ultimately, more timely discharge home. Selected components of the protocol are outlined in the table below.
Advertisement
Other additions to the protocol that have helped decrease length of stay include:
Other perioperative techniques for reducing blood loss and allogeneic blood transfusions also show promise. The use of tranexamic acid, hypotensive anesthesia and intraoperative cell salvage has reduced our use of allogeneic blood transfusion to almost zero.
We are in the process of collecting specific data on this protocol, and the results since its inception in 2014 are promising. With the institution of this new protocol, average length of stay was reduced to 3.3 days in the first six months of 2015, with 67 percent of patients going home in three days or less.
Integration of the protocol into the electronic medical record helped make the transition seamless, and all three surgeons performing pediatric scoliosis surgery — including Thomas Kuivila, MD, and David Gurd, MD — are using the protocol essentially 100 percent of the time. Cost data are not yet available, but we anticipate a significant reduction in total hospital expenses through use of this protocol with no change in ultimate outcomes.
Preliminary patient satisfaction data are likewise promising, and we have seen no increase in emergency department visits for pain control following discharge. We also see no differences in perioperative complications. We anticipate no differences in fusion rates as well, although long-term data — which are not yet available — will be required.
Advertisement
While this protocol is in its infancy at our institution, it has significantly improved the efficiency of postoperative care delivery in this subset of patients. Further dedicated prospective studies on specific clinical outcomes and cost are forthcoming.
Dr. Goodwin is Director of the Center for Pediatric and Orthopaedics and Spine Deformity, Assistant Program Director for the Orthopaedic Surgery Residency, and Assistant Professor at Cleveland Clinic Lerner College of Medicine.
Advertisement
Advertisement

Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients

How to diagnose and treat crystalline arthropathy after knee replacement

Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network

Reduced narcotic use is the latest on the list of robotic surgery advantages

Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals

Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions