Endoscopic therapy safely treats strictures without balloon dilation or surgery

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1239c166-749f-4852-ba36-7d4405b32e2d/16-DDI-445-EndoNeedleKnife-CQD-650x450_jpg)
16-DDI-445-EndoNeedleKnife-CQD-650×450
Endoscopic therapy safely treats strictures without balloon dilation or surgery
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For most patients with inflammatory bowel disease (IBD), strictures are a painful reality. Surgically altering the anatomical structure of the bowel often leads to postoperative strictures and inflammation that narrow the intestine. To remove these strictures, patients typically have to undergo additional surgeries or balloon dilation. However, neither option is without risk of complications.
As leaders in digestive disease research, Cleveland Clinic physicians have discovered a new way to apply an established endoscopic technology to treat these strictures safely and effectively.
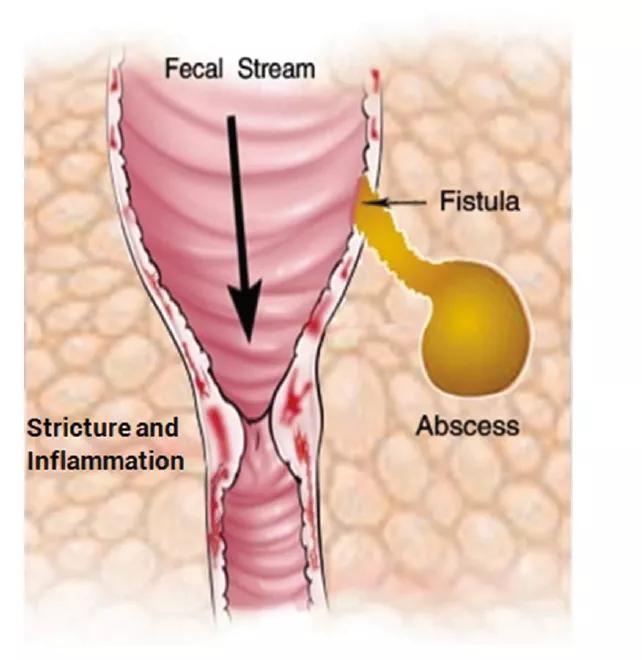
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/24e06f48-2452-47ff-bdbf-cf02780ef38a/Stricture-abscess-diagram_png)
Figure 1: Sketch model illustrating association between inflammation, stricture, fistula and abscess in the intestine.
Principle Investigator Bo Shen, MD, Section Head of Cleveland Clinic’s IBD Center, has demonstrated the application of endoscopic needle-knife stricturotomy to successfully treat strictures in the lower gastrointestinal (GI) tract. The results of this clinical research were presented today at Digestive Disease Week 2016.
Patients with ulcerative colitis or Crohn’s disease may develop strictures in the bowel as their condition progresses. Following a bowel resection, strictures and abscesses may form, causing abdominal pain, diarrhea, nausea, vomiting, weight loss and m
alnutrition. To alleviate these symptoms, surgery may be used to remove the affected section of intestine. However, this procedure further reduces the length of the intestine. Without additional medical treatment, 80 percent of patients will suffer disease recurrence.
Advertisement
Another method of widening the intestinal tract involves balloon dilation. Although it’s less invasive than surgery, it carries the risk of perforation of the intestinal wall and intern
al bleeding. In addition, balloon dilation only lasts about three months before the strictures return.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/512f01ee-66f5-480c-bdf6-e8d9acc85c4b/stricture_png)
Figure 2: Stricture being treated with a needle knife.
Dr. Shen wanted to find a safer, more effective way to treat strictures in the lower GI tract. With 17 years of experience in digestive disease management, he was alr
eady skilled in using endoscopic needle-knife technology to treat strictures in the upper GI tract. So he decided to see if that same FDA
-approved technology could be used in the lower GI tract.
To begin, Dr. Shen assembled a database of 63 patients who were diagnosed with strictures at Cleveland Clinic from 2008 to 2015. For most patients, he was able to use endoscopic needle-knife therapy to treat their strictures with excellent results. The youngest patient he treated was only 10 years old.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0fbe0961-be55-4c1e-8c04-e2672847606c/stricture-need_png)
Figure 3: Stricture after treatment with a needle knife.
“The beauty of the needle knife is that it can cut and cauterize at the same time, allowing the physician to cut the stricture that’s narrowing the bowel,” explains Dr. Shen. “This treatment lasts two to three times longer than balloon dilation and carries a much lower risk of perforation.”
How does endoscopic needle knife compare to surgery? “Finding alternatives to surgery is key for patients with IBD because each surgical procedure increases their risk of complications and recurrence,” explains Dr. Shen. “Each time we can avoid surgery, we’re preserving the patient’s intestinal tract and extending his or her quality of life.”
Advertisement
Dr. Shen has already started training physicians from Cleveland Clinic and around the world in the innovative application of this endoscopic technology.
“We’re happy to educate other physicians about our research and help them make this proven endoscopic technology the gold standard in treating strictures in the lower GI tract,” he says.
Advertisement
Advertisement
Strong patient communication can help clinicians choose the best treatment option
ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance
The importance of raising awareness and taking steps to mitigate these occurrences
New research indicates feasibility and helps identify which patients could benefit
Treating a patient after a complicated hernia repair led to surgical complications and chronic pain
Standardized and collaborative care improves liver transplantations
Fewer incisions and more control for surgeons
Caregiver collaboration and patient education remain critical