Investigators looked at nearly 3 million patients

Despite the fact that vasectomy is a simple, effective outpatient procedure, it is an underused form of birth control in the United States with only 8 to 12 percent of couples relying on it for family planning.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One thing that may be contributing to its low usage is the three-decade long debate over whether the procedure increases a man’s risk for prostate cancer. In the late 1980s and 1990s, several studies emerged showing a slight association between vasectomy and the risk of prostate cancer.
Now a recent meta-analysis published in July in JAMA Internal Medicine should finally end the debate, says Eric Klein, MD, urologist and Chairman of Glickman Urological and Kidney Institute at Cleveland Clinic. “It’s a very strong analysis and it puts it to rest once and for all: there is no increased risk of prostate cancer for men who have a vasectomy.”
The older studies that found a slight correlation between vasectomies and prostate cancer were small and single-institution or single-cohort studies. Even though they found an only slightly elevated risk, Dr. Klein says, it created anxiety in some men interested in vasectomies.
One of the constant criticisms of those studies was the argument that correlation is not causation. Critics pointed out the cascade effect: simply by having a vasectomy, a man was more likely to see a urologist in the future because he had a familiarity with the specialty. By seeing a urologist, he was then likely at some point to have a PSA test, which could lead to a biopsy and a cancer diagnosis.
“No one ever came up with a robust biological rationale or even a plausible one for why the two should be linked,” Dr. Klein says. “The challenge with epidemiological studies like this is you can’t infer causation. That would require a randomized controlled trial that frankly could never be done. This meta-analysis is the best evidence we are ever likely to have on this issue.”
Advertisement
The new meta-analysis looked at large group of patients and included studies that had different designs, including case, cohort and cross-sectional studies. “It’s a very strong study,” Dr. Klein notes. “It’s the largest that’s ever been done and its strength lies in the number of participants, almost 3 million.
“When you ask a question over such a broad segment of the population, you’re going to get much closer to the truth than any individual study does. And what this study showed was that there is no increased risk of getting prostate cancer if you had a prior vasectomy. That should set everyone’s mind at ease.”
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
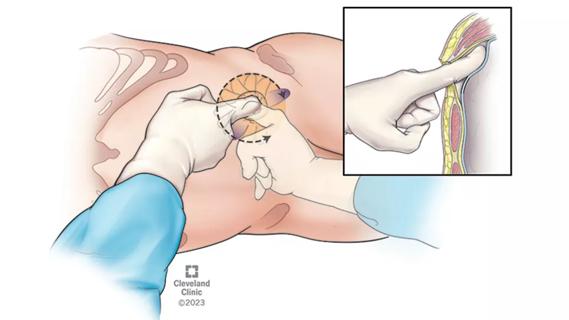
Pioneering and refining the approach in pyeloplasty, nephrectomy and more
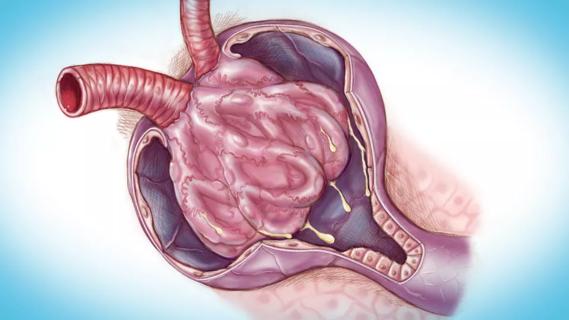
Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
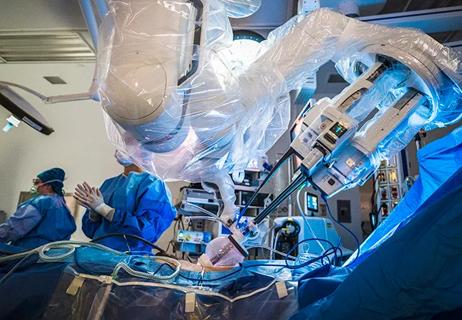
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients