Scott Cameron, MD, PhD, also brings wide-ranging research interests to bear

Scott Cameron, MD, PhD, has been named to lead the Section of Vascular Medicine at Cleveland Clinic, the largest vascular medicine program in the United States. “It’s an honor,” says Dr. Cameron. “I’m looking forward to making it possible for our section’s physicians and other caregivers to do their best work.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In some places, vascular medicine may be underappreciated. But at Cleveland Clinic the program has long been recognized for excellence in thrombosis and esoteric vascular disorders. “I want to preserve this reputation,” Dr. Cameron says, “and increase the breadth of services our section offers.” Just as the vascular system links every organ in the body, he notes, vascular medicine specialists are well positioned to collaborate for better patient care with a broad range of medical and surgical specialties.
Born in Scotland, Dr. Cameron studied pharmacology at the University of Edinburgh and came to the United States two decades ago with “two thousand dollars, two suitcases and a one-way ticket.”
He earned a doctorate in pharmacology at the University of Rochester and trained as a fellow in clinical chemistry at Johns Hopkins Hospital. He went on to take a medical degree at SUNY Upstate Medical University, did an internal medicine residency at New York Presbyterian Hospital, and completed a five-year clinical and research fellowship in cardiology and vascular medicine at the University of Rochester. His investigative interest in blood vessel disease deepened at every stage of his education and training.
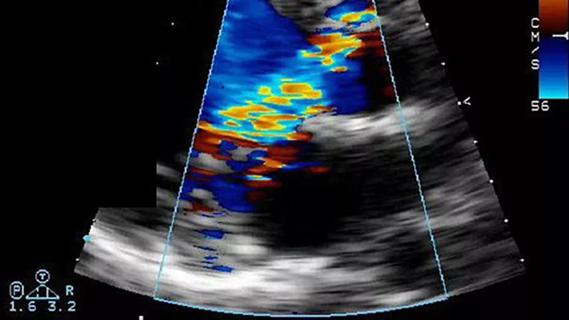
“Most of my research was vascular in nature, so cardiovascular disease was a natural fit,” he explains. “I gained subspecialty certification in vascular medicine and vascular ultrasound as well as cardiovascular disease to better align my clinical work with research interests.”
Dr. Cameron joined Cleveland Clinic in 2019 and was tapped to lead the Section of Vascular Medicine upon the retirement of longtime section head John Bartholomew, MD, earlier this year. A strong advocate of Cleveland Clinic’s “team of teams” approach, Dr. Cameron is eager to collaborate with colleagues in the institution’s Miller Family Heart, Vascular & Thoracic Institute and beyond.
Advertisement
“This is an exciting time to be heading up Cleveland Clinic’s vascular medicine program,” he says. “We have a critical mass of experienced veterans and young talent. Our training program is one of the nation’s largest, and we hope to make it even larger. Overall, my goal is to make this a hot spot for patients, fellows and referring physicians from around the world.”
“With Dr. Cameron’s leadership, our talented and accomplished group of vascular medicine specialists will reach new heights in the clinical and academic arenas,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine.
Cleveland Clinic’s Section of Vascular Medicine was founded in 1947, initially as the Department of Peripheral Vascular Disease. In 2001, the program merged with the cardiology program to become the Department of Cardiovascular Medicine.
A cardiologist himself, Dr. Cameron believes that cardiology and other specialties benefit from greater familiarity with vascular medicine. “About one-third of patients with coronary artery disease also have overt or occult peripheral vascular disease that may be easily overlooked,” he notes. “Vascular medicine specialists are trained to recognize subtle manifestations of vascular disease in unusual clinical contexts, including conditions that present as mystery diseases.”
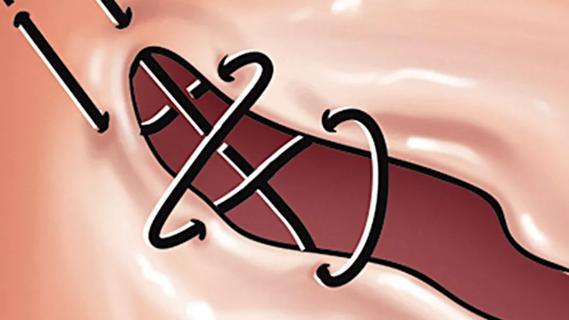
A prolific researcher, Dr. Cameron has focused his investigations on blood platelets, their changeable phenotypes and their effect on the vascular environment. He and his team found that platelets change their phenotype in diseases such as heart attack and peripheral artery disease. These “reprogrammed” platelets do not respond as predicted to medications, which may account for the heterogeneity of patient response to anticoagulants and antithrombotics.
Advertisement
The Cameron team helped establish that platelets are like circulating messengers, carrying information back and forth between blood vessels and organs. “A major goal of my research is to understand the process of platelet reprogramming and identify additional proteins on platelets which could be targets for new medications,” he says, adding that the ultimate objective is more-personalized treatment for vascular disease.
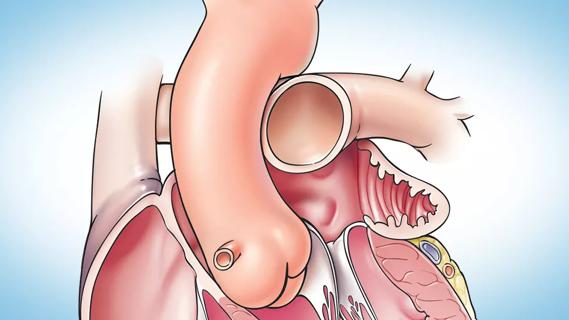
Aortic aneurysms are another of Dr. Cameron’s research interests. As a trainee, he was troubled to witness patients die of ruptured abdominal aortic aneurysms after being mistakenly diagnosed with heart attacks. As a cardiac ICU attending a few years later, he was able to pull one such patient from the brink by performing a bedside abdominal ultrasound in the emergency department despite an ECG pattern consistent with acute heart attack. “The patient’s blood pressure was too low, he looked like he was about to die and he insisted this was the worst abdominal pain he’d ever experienced,” he explains. “The surgeon who ultimately saved the patient arrived within four minutes because he had been a research mentee in my lab and we had a high level of mutual trust, frequently calling on each other in emergencies. This is the type of collaborative and multidisciplinary spirit to improve care that I see here at Cleveland Clinic and that I aim to promote even further.”
Cases like that spurred Dr. Cameron to pursue investigations that he hopes may one day yield a medical therapy for aneurysms. Working with cardiothoracic and vascular surgery colleagues, he has learned that aneurysms and platelets react to one another in a kind of loop that contributes to blood vessel remodeling. They have also identified a platelet receptor that could be a druggable target in patients with aneurysms. “The potential impact of this project is broad and involves classical biochemistry, pharmacology, molecular genetics and physiology, as well as advanced imaging modalities,” he concludes.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
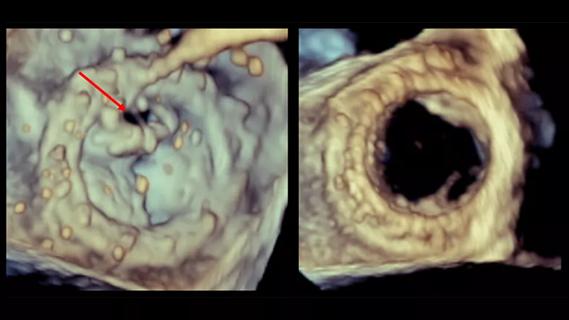
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
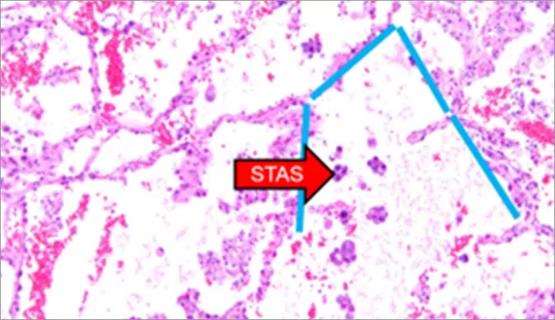
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable