A shift from single-modality evaluation to real-world clinical decision-making
For the first time, a group of experts has detailed appropriate combinations of imaging modalities for the assessment of nonvalvular heart disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The recommendations come in the form of new appropriate-use criteria (AUC) from the American College of Cardiology (ACC) in collaboration with nine other cardiology and cardiothoracic surgery societies. The AUC document, published in the Journal of the American College of Cardiology (2019;73:488-516), is the second set of recommendations to come from a multiyear collaboration among the societies to provide guidance on multimodal imaging of the heart in various clinical settings. It’s a companion to a 2017 AUC document on valvular heart disease that was reported on in a previous Consult QD post.
The aim of the AUC documents is to shift from evaluating single imaging modalities in favor of a more diagnosis-oriented approach aimed at identifying multiple imaging tests that may be appropriate for a given indication.
“This approach more accurately mirrors a clinician’s thinking process and provides a consensus-based rubric to support cardiac screening and diagnosis,” explains Cleveland Clinic heart failure cardiologist and Heart Failure Society of America president Randall C. Starling, MD, MPH, who served as a rating panel member for the new AUC document. Among his colleagues on the AUC rating panel was Cleveland Clinic cardiovascular imaging specialist and professor of radiology Paul Schoenhagen, MD, who also served on the five-member writing group for the document.
The process began with a small team of experts in imaging and nonimaging fields plotting indications for imaging in nonvalvular heart disease (symptoms and diagnoses) against imaging tests across multiple modalities. Then a review panel of various subspecialists and generalists provided clarification on the clinical scenarios. Finally, the rating panel assigned values to the appropriateness of each modality for each scenario. A scale of 1 to 9 was used, with 1 to 3 being “appropriate,” 4 to 6 indicating “may be appropriate” and 7 to 9 signaling “rarely appropriate.” The result is a tricolor chart covering more than 100 indications, with green, yellow and red cells designating recommendations on appropriateness of use.
Advertisement
“It was a labor-intensive process, but it resulted in a wide-ranging, comprehensive document that offers solid guidance while still acknowledging the gray areas that legitimately exist,” notes Dr. Starling, who is also Professor of Medicine at Cleveland Clinic Lerner College of Medicine.
“The resulting criteria offer guidance for both initial evaluation and sequential or follow-up testing to clarify diagnoses, monitor ongoing conditions and investigate worsening symptoms,” adds Dr. Schoenhagen.
Additional sections of the AUC document offer guidance on device imaging (see example in Figure below), evaluation for closure of patent foramen ovale and atrial septal defects, evaluation for stroke/transient ischemic attack, and intraprocedural guidance and assessment in left atrial appendage occlusion procedures.
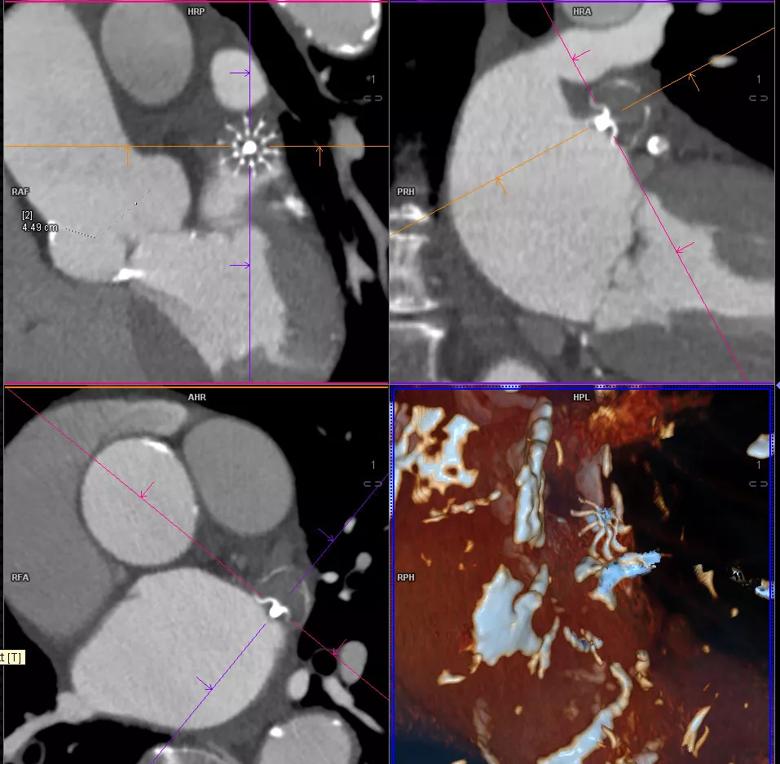
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6bcf5e0c-1b9c-4fac-a6bd-dde32ef4a55e/19-HRT-034-watchman-inset_jpg)
Figure. CT images from a patient with prior placement of the Watchman® left atrial appendage (LAA) closure device. The left lower and right upper panels show the device in the LAA in oblique four-chamber and two-chamber views, respectively. The left upper panel shows the device “en face,” and the right lower panel shows a volume-rendered image with the device in the center.
To provide easy access for physicians, clinical decision support tools, translated from the AUC document, are being developed for integration into an EHR or radiology ordering portal. These tools aim to translate content to true/false, machine-readable, automated logic.
“Clinicians who read the AUC carefully will find most of it is common sense to them,” Dr. Starling observes. “The tricky part is that some of these imaging modalities are fast-evolving. Depending on how specialized your practice is or how current your knowledge may be, some scenarios, such as those involving specialized techniques with intracardiac echocardiography, may not be familiar to all cardiologists.”
Advertisement
Costs of imaging tests were not a consideration in determining ratings. “Generally, as long as an appropriate test for the indication is ordered, the AUC document can be used to support reimbursement of the test’s customary cost,” Dr. Schoenhagen says.
Nevertheless, different locations differ in their levels of equipment, technology and expertise. “Physicians in remote rural locations may have two options for a scenario while I have four options to choose from at Cleveland Clinic,” Dr. Starling notes. “They will have to justify the imaging test they choose, based not only on the AUC but also on which tests they have the capacity to conduct.”
Dr. Schoenhagen adds: “You could make an argument to image with CT or MRI depending on at least three factors — what is locally available, where you have local expertise and the characteristics of the patient.”
Development of these AUC documents could not have come too soon, Dr. Schoenhagen adds. “The use of imaging in general has increased over the past decade,” he says. “Payers want to ensure that the use of imaging is optimized, in the sense of both clinical results and cost-effectiveness.”
To that end, the AUC developers strove to close gaps that payers might otherwise fill with their own reimbursement parameters. “The ACC is a proactive organization that forms advisory boards, fosters collaboration and generates information so that the physician community is determining best practices,” says Dr. Starling. “The ACC has done an excellent job of garnering the trust of organizations that set ground rules for when and how imaging studies are reimbursed.”
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable