Randomized control trials support surgery’s role in managing blood sugar
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
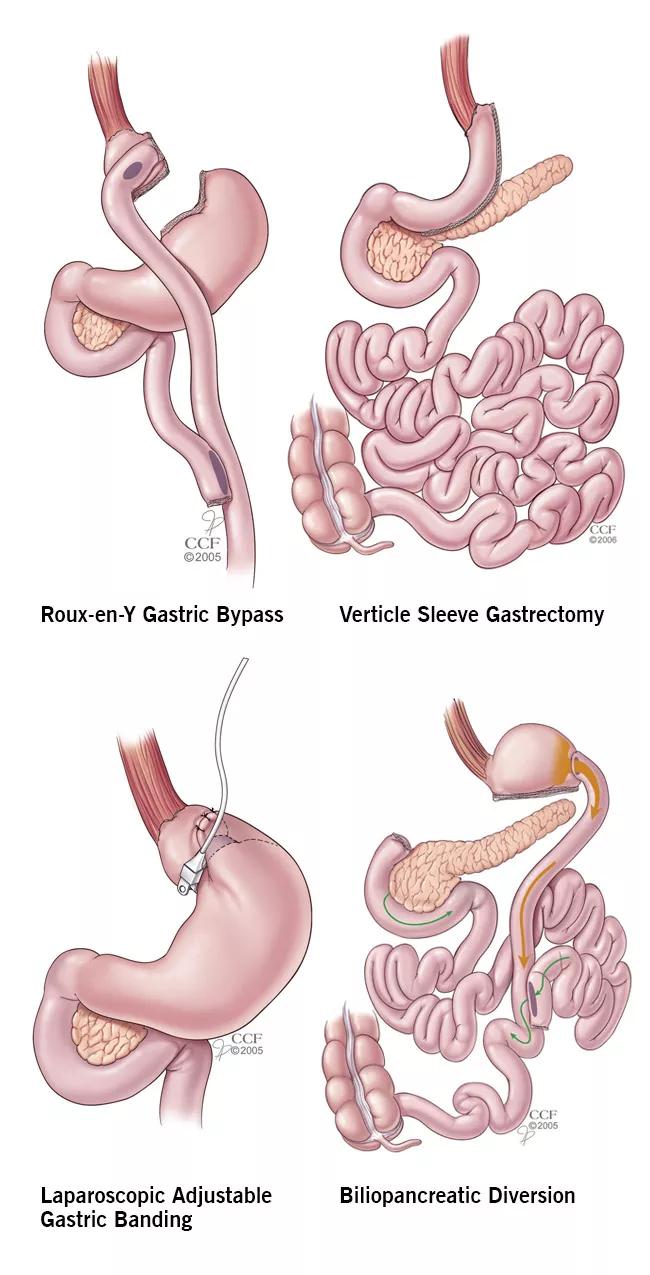
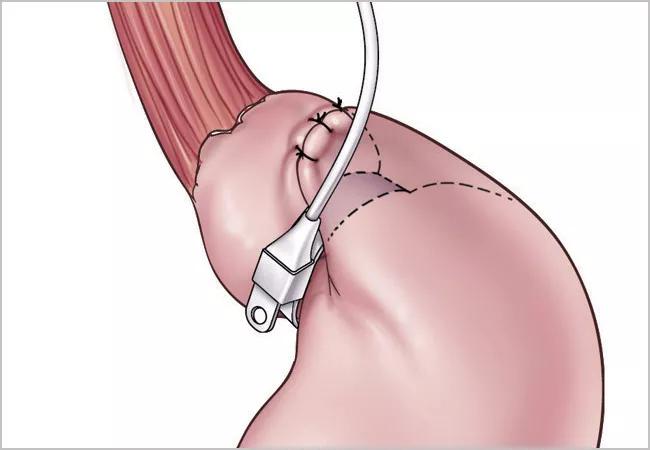
Figure 1: Diagrams of the four bariatric operations currently in common clinical use.
Physicians around the world recognize diabetes as a global health crisis. The International Diabetes Federation reports that 415 million people around the world have this condition. The vast majority of these patients have type 2 diabetes mellitus (T2D). Unfortunately, fewer than half of adults with T2D successfully control their blood sugar with medication and lifestyle interventions, according to Diabetes Care.
Until recently, bariatric surgery was not considered a standard treatment option for patients with T2D. Thanks to recent clinical trials, including the STAMPEDE trial conducted by Cleveland Clinic, the American Diabetes Association has published new guidelines to validate the efficacy of bariatric surgery and regulate its usage in diabetics with lower BMI thresholds. These guidelines are designed to help physicians get their patients with T2D in control of their condition when medication and lifestyle changes have failed.
For the past 10 years, health experts from around the world have been working to clearly define the role of surgery in the treatment of diabetes. Philip Schauer, MD, Director of Cleveland Clinic’s Bariatric and Metabolic Institute, led clinical trials designed to compare the efficacy of surgery versus medication and lifestyle interventions. Of the clinical trials conducted, the STAMPEDE trial was the largest randomized control trial.
“Before 2007, there were almost no randomized control trials in this field,” reveals Dr. Schauer. “Now we have results from 11 randomized control trials that demonstrate bariatric surgery’s superiority to medical therapy. This research has significantly improved the quantity and quality of evidence needed to enhance diabetic treatment algorithms.”
Advertisement
The new clinical guidelines for diabetes care include about 30 recommendations endorsed by 45 global diabetes medical and surgical organizations. The following modified BMI thresholds allow patients with mild obesity to qualify for surgical intervention before developing serious diabetes-related complications:
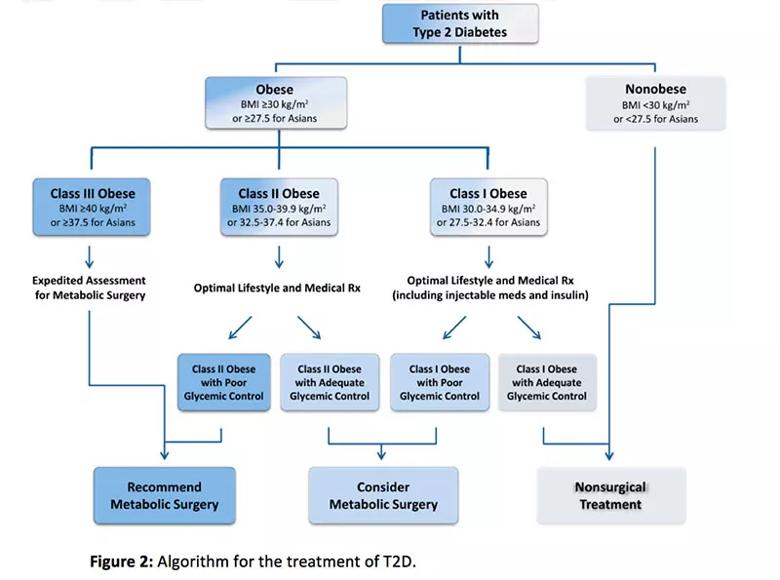
Figure 2: Algorithm for the treatment of T2D.
The new guidelines help educate patients and doctors on bariatric surgery and the ways to minimize risks when using it to treat T2D. By including surgery as part of a comprehensive treatment program, doctors and surgeons can safely care for all the medical needs of the patient.
In addition to education, the new guidelines have financial benefits for patients. As more commercial insurance companies review the new standards for diabetes treatment, they’ll be encouraged to provide full coverage for patients with lower BMIs so that they can get the financial support needed to undergo bariatric surgery.
“Prior to the new guidelines, physicians only had two strategies for treating T2D: drugs and diet/exercise,” explains Dr. Schauer. “Now doctors have a third evidence-based method — surgery — to help patients achieve superior glycemic control and reduce their risk of heart attack, stroke, blindness and renal failure.” The new guidelines may even help patients with T2D achieve remission (normal blood sugar without medications) if surgery is used early in the course of disease progression.
Advertisement
Advertisement

Strong patient communication can help clinicians choose the best treatment option

ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance

The importance of raising awareness and taking steps to mitigate these occurrences

New research indicates feasibility and helps identify which patients could benefit

Treating a patient after a complicated hernia repair led to surgical complications and chronic pain

Standardized and collaborative care improves liver transplantations

Fewer incisions and more control for surgeons

Caregiver collaboration and patient education remain critical