Also better reflects actual clinical scenarios

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e97f26bd-cdf9-4a25-bced-5200199bfa2b/14-ORT-1695-Kolmodin-Hero-Image-690x380pxl_jpg)
14-ORT-1695-Kolmodin-Hero-Image-690x380pxl
By Joel Kolmodin, MD, and Paul Saluan, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteochondritis dissecans (OCD) of the elbow is increasingly prevalent in the U.S. pediatric population, particularly in young throwing athletes such as baseball players. The condition is thought to be secondary to repetitive compressive and shearing forces exerted by the radial head on the humeral capitellum during the throwing motion. These forces have been shown to cause microtrauma of the articular cartilage, leading to avascularity, fracturing and ultimately overt detachment from subchondral bone. Traumatic cartilage changes invariably lead to the insidious onset of pain and functional limitation, often accompanied by mechanical symptoms and significant loss of motion in advanced lesions.
Treatment options for capitellar OCD lesions are numerous, ranging from simple rest to arthroscopic debridement and drilling, fragment fixation, and autograft or allograft transfer. All management options can be successful when used in the appropriate clinical scenario.
Since its publication in 2007, the Takahara classification for pediatric OCD lesions of the capitellum1 has proved to be a valuable tool for guiding management of OCD lesions. The classification establishes two groups of patients:
Stable lesions were defined as those that occur in a capitellum with an open physis, display low-grade radiographic changes and have maintained elbow range of motion (ROM). Conversely, unstable lesions were defined as those that are found in a capitellum with a closed physis, display higher-grade radiographic changes and have restriction of elbow motion greater than 20 degrees.
Advertisement
It is generally accepted that stable lesions can be effectively treated nonsurgically, but surgical decision-making regarding unstable lesions has not been fully elucidated. While the Takahara classification system has proved very useful in guiding the decision to pursue nonoperative over operative management, it does not include discrete guidelines to direct surgical management based on lesion characteristics. One key element not accounted for in the classification scheme is lesion location on the capitellum, which is increasingly recognized as having significant implications in surgical management.
Past cadaveric biomechanical studies have demonstrated that capitellar valgus laxity and contact pressures increase in the presence of capitellar OCD lesions and that these contact pressures are greater in lateral defects than in central defects. Similarly, many clinical studies have demonstrated that lateral lesions tend to be associated with more severe symptoms and loss of function. Much better outcomes are seen when lateral lesions are treated with aggressive surgical interventions such as autograft reconstruction.
In view of this evidence, we have proposed and published a refinement of the Takahara classification for OCD lesions of the elbow (Table).
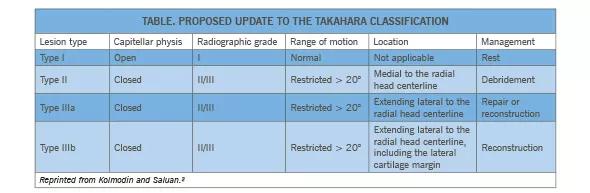
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c943b8b0-a65d-4c3c-81cd-894dde3dfa73/Table-from-14-ORT-841_jpg)
This modification is based on the location of the lesion on the capitellum, as determined on a 45-degree flexed, supinated view of the elbow (Figures 1 and 2). The capitellum is divided into two halves, defining medial (type II) and lateral (type III) lesions. Radiographic grade is assessed using the Minami classification.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5f92700b-dced-4c76-9921-9d20561e3de2/14-ORT-1695-Kolmodin-Inset-Image-590pxl-width_jpg)
Figure 1. (left) A 45-degree flexed, supinated anteroposterior X-ray view of an elbow with type II (medial) and type III (lateral) OCD lesions. Reprinted from Kolmodin and Saluan.2. Figure 2 (right). X-ray of an elbow with a type IIIb OCD lesion. Reprinted from Kolmodin and Saluan.
Type I lesions (“stable”) have an open capitellar physis, grade I radiographic findings and nearly full ROM at the time of diagnosis. Most of these lesions heal completely if treated with thorough rest.
Type II lesions (“unstable”) are those with a closed capitellar physis, a grade II/III radiographic profile or presentation with restricted elbow ROM, and a location medial to the radial head centerline. These lesions tend to respond well to simple debridement or repair.
Type IIIa lesions (“unstable”) have a closed capitellar physis, grade II/III radiographic findings or presentation with restricted elbow ROM, and a location lateral to the radial head centerline. They tend to do better with more aggressive therapies, such as repair or reconstruction.
Type IIIb lesions (“unstable”) are those with a closed capitellar physis, a grade II/III radiographic profile or presentation with restricted elbow ROM, and a location lateral to the radial head centerline, including the lateral cartilage margin. These lesions require reconstruction, which enhances stability and reduces shear forces experienced by the lateral capitellum.
We believe that our update to the Takahara classification, by accounting for lesion location, better reflects the clinical scenarios physicians are encountering and the current questions being addressed in the literature. We anticipate that our updated classification scheme will improve the way capitellar OCD lesions are characterized and systematically treated and will help guide surgical management more effectively and shape further research efforts.
Advertisement
Dr. Kolmodin is a fourth-year orthopaedic surgery resident in the Department of Orthopaedic Surgery.
Dr. Saluan is a surgeon with the Center for Pediatric Orthopaedics and Cleveland Clinic Center for Sports Health in the Department of Orthopaedic Surgery
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions