Diagnosis and treatment depend on clinical manifestations, which vary widely
The clinical manifestations and course of sarcoidosis vary, in part because the tiny collections of granulomas associated with this chronic disease can occur in any part of the body. The most common manifestations of neurosarcoidosis, which affects approximately 5% of sarcoid patients, include cranial neuropathy, polycranial neuropathy and meningitis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Conducting a systemic evaluation to find a biopsy target is essential when trying to diagnose sarcoidosis, says Brandon Moss, MD, a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis who also sees patients in its Sarcoidosis Center. “As they say, tissue is the issue,” he notes, “so the main job is to try and get biopsy proof of granulomatous disease.”
In the newest episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Moss discusses neurosarcoidosis, the complexity of its differential diagnosis and other management issues. He delves into:
Click the podcast player above to listen to the episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
Dr. Moss: In terms of a gold standard for diagnosis for neurosarcoidosis, right now I think the most established is the Neurosarcoidosis Consortium Consensus Criteria for the Diagnosis of Sarcoidosis. These are largely based on the Zajicek criteria, which have been around for a much longer period of time. But essentially, everybody needs to have a clinical presentation and diagnostic evaluation that suggests neurosarcoidosis. And the diagnostic evaluation should include studies that are pertinent for that disease manifestation, whether it’s MRI, spinal fluid studies or EMG nerve conduction studies.
Advertisement
There should also be a thorough workup for mimics for everybody, to make sure you’re not missing some of these key players, which could also be in the differential diagnosis. After that, the diagnosis is dependent upon biopsy, and there are various levels of certainty depending upon whether or not you can get a biopsy showing granulomatous disease [see image below] and where the biopsy is. So people with possible sarcoidosis do not have biopsy evidence of granulomatous disease. People with probable neurosarcoidosis have biopsy evidence of sarcoidosis in a non-neural organ system. And people with definite neurosarcoidosis have biopsy proof of granulomatous disease within the nervous system.
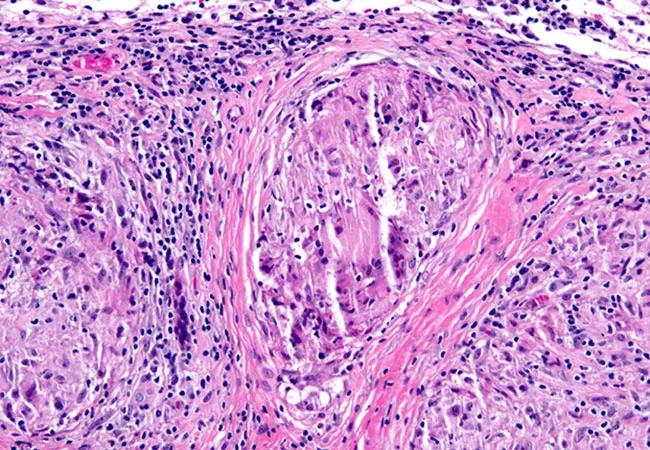
Pathology image showing a granuloma in the meninges, the key identifying feature of neurosarcoidosis.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade