Insights on a fast-growing subspecialty area
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The past decade has seen a dramatic expansion in our understanding of immune-mediated neurological disorders involving both the central and peripheral nervous systems. Neurological dysfunction arises as a result of disease-specific autoantibodies generated against receptors or transporters involved in central or peripheral nervous disease function.
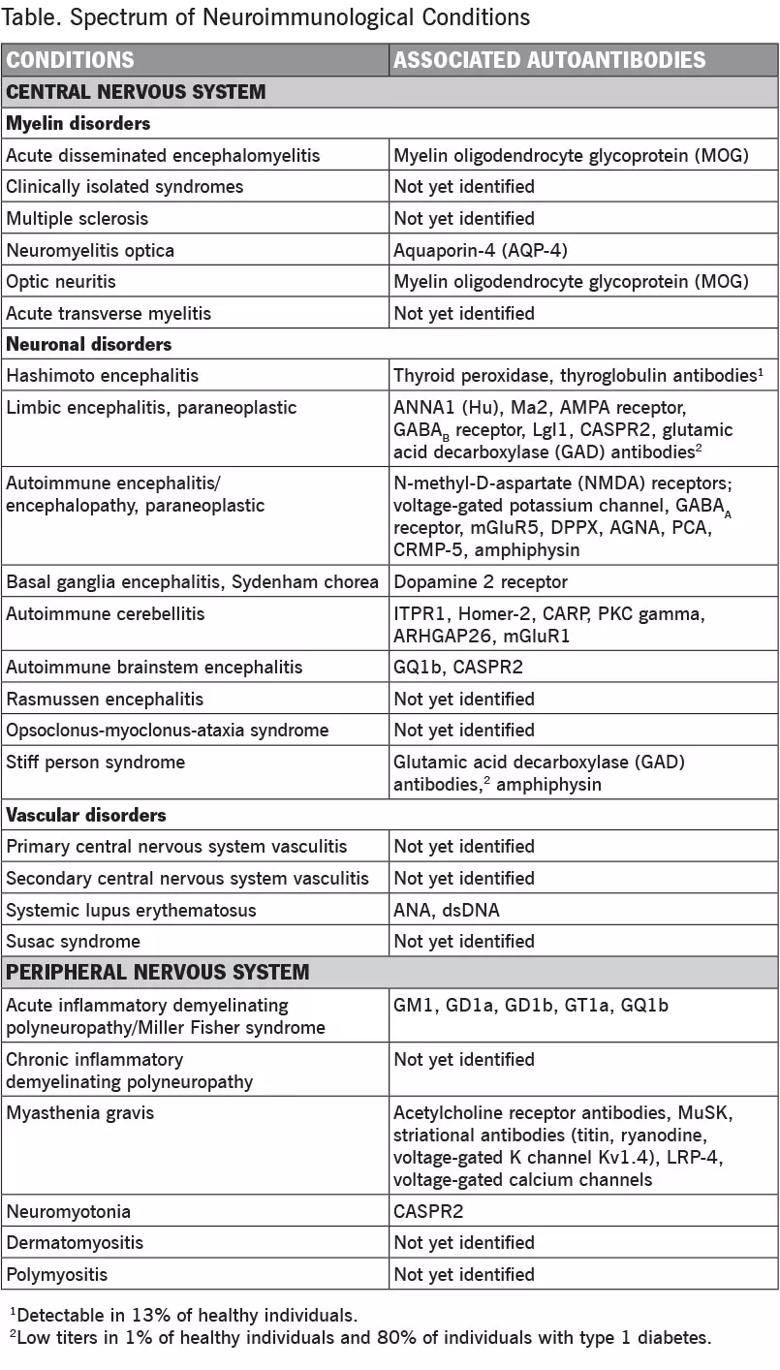
Increasingly, these disorders are being recognized in children and involve unexpected disease processes such as encephalopathies, epilepsies, movement disorders, channelopathies and paraneoplastic syndromes (Table).
While the pathogenic importance of some of these antibodies has clearly been demonstrated, other autoantibodies appear more likely to be epiphenomena and require further study. For example, autoantibodies to glycine receptors, NMDA receptors or voltage-gated potassium channel-associated proteins occur in up to 11 percent of individuals with “idiopathic” epilepsy, although usually at much lower titers than those seen in patients with forms of autoimmune encephalitis, and it is unclear whether the autoantibodies contribute to disease (Crisp et al. Nat Rev Neurosci. 2016;17:103-117). Additionally, there are a number of brain immune-mediated disorders for which an autoantibody is suspected but has not yet been identified (e.g., opsoclonus-myoclonus-ataxia syndrome).
Early recognition is critical to ensure appropriate management of these potentially treatable diseases. Therapeutic options have significantly expanded over the past few years with the introduction of a number of biologic response modifiers or “biologics” (large, complex molecules produced using recombinant DNA technology) designed to both prevent disease progression and treat symptoms.
Advertisement
Neuroimmunology’s increasing importance is further underscored by the fact that numerous conditions are now recognized to have an immune/inflammatory component, from the association of infection/inflammation in periventricular leukomalacia in the preterm infant to Alzheimer’s and Parkinson’s disease at the other end of the age spectrum. Immune activation of the central or peripheral immune system plays a key role in the pathogenesis of many neurological disorders. Recent studies, for example, have shown that NMDA receptor encephalitis in children is more common than any other specific infectious encephalitis and is not necessarily associated with tumors. Research using immunotherapy antibodies to treat glioblastoma multiforme is another example.
For these reasons, a comprehensive understanding of the relationship between the nervous and immune systems is crucial for practicing pediatric neurologists in the 21st century. With the increasing prevalence of these disorders and maturation of the field, neuroimmunology is rapidly becoming a recognized pediatric neurology subspecialty area.
Cleveland Clinic Children’s Neuroimmunology Program takes a collaborative, interdisciplinary approach to the care of patients with these disorders that often involve multiple organ systems, drawing on the expertise of pediatric neurologists, rheumatologists, oncologists, endocrinologists and others. For a sampling of that caregiving, I refer you to recent case studies published on this blog by several of my colleagues, including cases of encephalitis, acquired demyelinating disease and temporal lobe epilepsy — all with immune-mediated components. We welcome your comments as well as inquiries about opportunities to collaborate on the management of particularly challenging cases.
Advertisement
Dr. Friedman (friedmn@ccf.org) is Director of the Center for Pediatric Neurosciences in Cleveland Clinic Neurological Institute and Cleveland Clinic Children’s.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade