Misdiagnosis is common in this population
By Manikum Moodley, MBChB, FCP, FRCP
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Multiple sclerosis (MS) is primarily an autoimmune demyelinating disease of young adulthood, with a clinical onset typically occurring between 20 and 40 years of age.
However, it is now being recognized with increasing frequency in children and adolescents. The first descriptions of MS in children were recorded in the early 19th century, but recently improved awareness of this disease and subspecialty training in pediatric MS have allowed early and accurate evaluation and easy access to appropriate comprehensive care.
The youngest age of onset of MS in the medical literature is 2 years but the majority of children are diagnosed in their early teens.1 In 3 to 5 percent of cases, MS onset is before age 16; an onset before 10 years of age is extremely uncommon, with a reported incidence of 0.2 to 0.7 percent.2
With its protean clinical manifestations and lack of biological markers, MS is easy to misdiagnose in adult patients. In children, correct diagnosis is an even greater problem because MS is uncommon and the various genetic and neurometabolic disorders produce active neurological impairment and white matter changes on MRI that mimic MS.
The burden of MS in the young is substantial. Younger children with MS present with multifocal and sometimes encephalopathic symptoms, making it difficult to distinguish MS from acute disseminated encephalomyelitis (ADEM).3 Children also tend to present with larger and tumefactive lesions, adding to the disease burden. Early-onset MS has an unfavorable outcome with frequent relapses at shorter disease-free intervals.4
Advertisement
There are extremely few case reports on the incidence of MS in very young children. Ruggerri et al.2,3 in Italy and Duquette et al.4 in Canada have published the few case series that have widened our horizon for further exploration of MS in the very young. Their publications outline the course and unique clinical and radiological features of MS in early childhood and its implications at later ages.
Cleveland Clinic’s youngest pediatric patient with MS recently presented to the Pediatric MS and White Matter Disorders Clinic at the age of 2 years 8 months for a second opinion on relapsing-remitting white matter disease, first detected at 2 years 1 month of age.
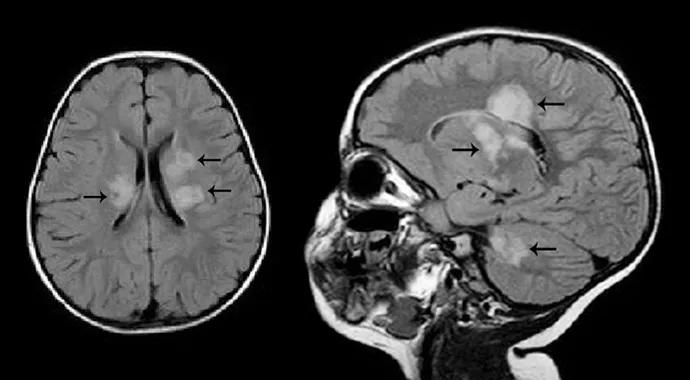
She had initially presented to another hospital for investigation of an acute onset of ataxia. Her brain MRI revealed extensive demyelinating white matter lesions involving bilateral corona radiata, white matter adjacent to the atria and right frontal horn, bilateral temporal lobes and the subcortical white matter (Figure 1).
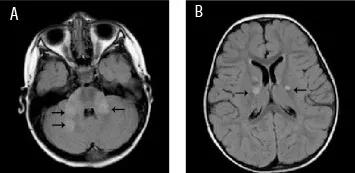
Figure 1. MRI brain (January 2011). T2 FLAIR axial images with black arrows demonstrating (A) Bilateral white matter lesions in the cerebellum, and (B) bilateral white matter lesions in the periventricular regions.
Ophthalmologic and cerebrospinal fluid (CSF) studies were normal. She was diagnosed with ADEM and treated with high-dose intravenous methylprednisolone (30mg/kg/day) for three days, followed by an oral steroid taper over six weeks.
She was readmitted with similar symptoms at two and four months after her initial presentation. Her repeat brain MRI revealed new areas of demyelination during each new admission (Figure 2). Her ophthalmologic examination, CSF studies and MRI spine were normal. At both of these presentations she was treated with high dose intravenous methylprednisolone for three to five days followed by a long oral steroid taper. Her physical examinations at these presentations were normal.
Advertisement
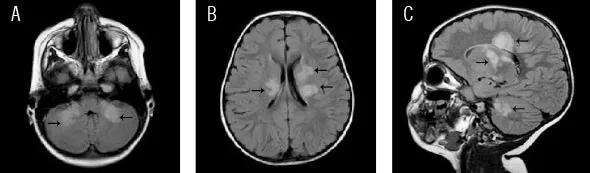
Figure 2. MRI brain (March 2011). T2 FLAIR axial images with black arrows demonstrating (A) Resolving bilateral cerebellar white matter lesions, (B) new white matter lesions in the periventricular regions, and (C) new pericallosal and cerebellar white matter lesions.
Seven months after the initial presentation, she was seen at the Pediatric MS and White Matter Disorders Clinic for a second opinion on diagnosis and management. Her workup included a repeat MRI brain and spine scan with and without contrast that revealed new foci of acute demyelination (Figure 3); CSF analysis revealed elevated myelin basic protein but negative oligoclonal bands, immunoglobulin index and neuromyelitis optica antibody. Extensive metabolic and thyroid studies were nonrevealing. Her clinical presentation with multiple relapses at two, four and seven months with new radiologic demyelinating lesions validated the diagnosis of MS, but her parents refused disease modifying therapy.
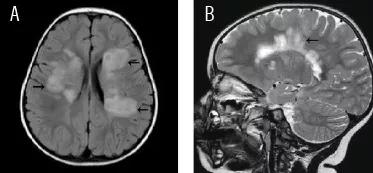
Figure 3. MRI brain (June 2011) T2 FLAIR axial images with black arrows demonstrating (A) extensive burden of demyelinating white matter lesions in the periventricular region, and (B) demyelinating plaques arranged perpendicular to the corpus callosum showing the typical Dawson fingers.
Diagnosing MS in the very young is medically and ethically challenging. The patient in the case in point was clinically asymptomatic after her second and third relapses but still demonstrated active demyelinating lesions on subsequent neuroimaging studies of the brain. MS in young children is significantly underdiagnosed, and this has important repercussions for treatment and long-term prognosis.
Advertisement
The majority of children initially present with a relapsing-remitting disease course and pose several challenges to the physician. In particular, the initial presenting clinical and radiological features may be difficult to distinguish from those of other congenital and acquired white matter diseases that have a higher prevalence in children than in adults, notably ADEM and metabolic and mitochondrial disorders.
This can lead to difficulties in establishing an early and accurate diagnosis and providing appropriate management.5 As there is now robust evidence that children with MS tolerate and may benefit from disease-modifying therapies, it is important to diagnose pediatric MS early and accurately so that the risk of developing major motor disability and cognitive impairment early in life can be significantly reduced.
Dr. Moodley is a neurologist in Cleveland Clinic’s Center for Pediatric Neurology. His specialty interests include pediatric multiple sclerosis, ADEM and other white matter disorders; pediatric neuromuscular diseases; neurofibromatosis; neonatal neurology; and pediatric autonomic disorders.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade