Study is first to confirm Cleveland Clinic’s approach to treating severe cases of acute ischemic stroke.
A major study from the Netherlands has demonstrated the effectiveness of using endovascular therapy to treat patients with acute ischemic stroke caused by intracranial arterial occlusion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
MR CLEAN (a Multi-center Randomized Clinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands) showed that when given within 6 hours of the onset of a stroke, intra-arterial treatment using a catheter, added to intravenous tissue plasminogen activator (tPA), was more effective than IV tPA alone, the current standard treatment. The 500 patients studied had acute ischemic stroke with a proximal intracranial arterial occlusion.
Results of MR CLEAN were presented in October at the 9th World Stroke Congress in Istanbul, and the study has been published online by the New England Journal of Medicine.
“This is really the first study that has shown us that this catheter-based treatment does have a benefit on top of standard medical treatment,” says M. Shazam Hussain, MD, head of the Cleveland Clinic Stroke Program. “That’s what makes it very exciting. The results confirm some of the practices that we’ve been advocating for some time, and support our current approach to treating these patients.”
Patients in the study had occlusions in the intracranial part of the carotid artery or the first part of either the middle cerebral or anterior cerebral artery, Dr. Hussain says.
“The concern with intravenous tPA is that, although it’s a very effective medication, when you have a very large clot sitting in a blood vessel like the carotid artery, the tPA circulates through the blood and has to eat away at this clot. The larger the clot, the harder it is to dissolve.”
Advertisement
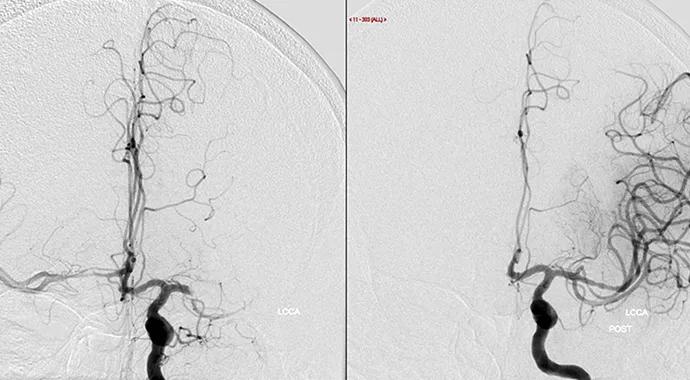
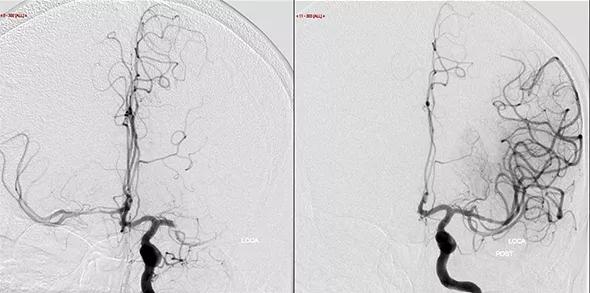
The endovascular approach involves threading a catheter from a puncture in the groin area to the occlusion and either administering medication directly to the clot or removing the clot with a device such as a retrievable stent. Mechanical removal (thrombectomy) is far more common than treatment with a thrombolytic agent, Dr. Hussain says.
The MR CLEAN patients were randomized to an intervention group, which received standard stroke therapy plus arterial catheterization, or a control group, which received standard therapy only. Patients were assessed after 90 days using the modified Rankin Scale (mRS) score, which evaluates functional ability on a scale of 0 to 6.
“A score of 0 is normal; scores of 1 or 2 indicate mild disability,” Dr. Hussain says. “A good outcome is considered to be a score of 0 to 2. After 90 days, 32.6 percent of patients in the interventional arm had an mRS score of 0 to 2, compared to 19.1 percent in the control arm. That’s a statistically significant difference between the two groups.”
The MR CLEAN results should prompt a new look at how stroke care is organized, Dr. Hussain says. “We’ve had a tendency to lump all stroke patients together in one group. Really, separating out these proximal vessel occlusions as a different type of group that requires a different treatment, I think, is important.”
Because patients with proximal occlusions generally present with more severe stroke symptoms, such as paralysis on one side or difficulty speaking, paramedics could be instructed to take those patients to centers that offer endovascular therapy, he explains.
Advertisement
“Transferring patients between hospitals slows down the process a lot, and the data has shown that it can take about three hours to transfer a patient from a smaller hospital to one where endovascular treatment is available,” Dr. Hussain notes. “You’re losing 2 million brain cells per minute in a stroke, so three hours can add up to a lot of brain.”
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade