Surgeon volume matters, so let’s start acting like it
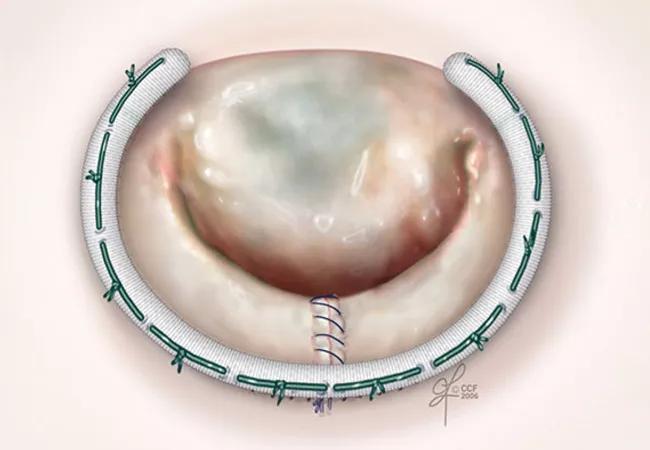
Is mitral valve repair a specialty? Yes, contend three Cleveland Clinic cardiothoracic surgeons in a recent editorial in the Journal of the American College of Cardiology (JACC).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The ‘jack of all trades’ cardiac surgeon represents an outmoded, unattainable ideal,” write the editorialists — A. Marc Gillinov, MD; Stephanie Mick, MD; and Rakesh Suri, MD, DPhil. “Excellence requires specialization,” they continue, noting that “[t]oday, trainees often choose to focus on particular areas within cardiac surgery: these include thoracic aortic disease, heart failure, congenital heart surgery, and transcatheter aortic valve replacement. Practicing surgeons should do the same…[and] mitral valve repair should be added to this list of specialties.”
Their editorial comes in the wake of an analysis of a mandatory New York State database published in JACC showing that cardiac surgeons who perform fewer than 25 mitral valve operations a year were significantly more likely to replace, rather than repair, mitral valves in patients with degenerative disease than were their counterparts who do 25 or more mitral valve surgeries a year. Patients of the lower-volume surgeons also had significantly worse survival and significantly higher reoperation rates compared with patients of high-volume surgeons.
The analysis focused on mitral valve repair rates because repair is established as conferring superior outcomes in degenerative mitral valve disease compared with replacement. The investigators, from the Icahn School of Medicine at Mount Sinai and Stony Brook University Hospital, found that operators with 10 or fewer mitral valve cases annually had a mean repair rate of 48 percent while those with more than 50 cases annually had a mean repair rate of 77 percent (P < .001).
Advertisement
The Cleveland Clinic editorialists note that “no examination of this topic has ever found…that surgeons’ volume or experience fails to influence repair rates and results. The weight of these data strongly supports the notion that valve repair for degenerative disease is a specialty.”
The editorialists go on to observe that this conclusion gives rise to two related questions of great import to patients and providers alike:
Advertisement
The Cleveland Clinic editorialists concede that while their recommendation for overt specialization in mitral valve repair will generate controversy, it is fundamentally a data-driven position. “Surgeon volume matters,” they conclude.
Read the full editorial by Drs. Gillinov, Mick and Suri here.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable