Case study illustrates key considerations
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 2011, a 66-year-old woman diagnosed with primary adenocarcinoma of the lung underwent a left lower lobectomy with video-assisted thoracoscopic surgery (VATS) at Cleveland Clinic. Her recovery was uneventful, and she subsequently stopped smoking. In 2015, she was diagnosed with an unrelated cancer in the remaining left upper lobe; this time, it was squamous cell carcinoma. Because her prior resection resulted in minimal scar formation in the chest (Figure 1), we were able to perform a completion pneumonectomy using VATS (Figures 2 and 3). Her postoperative course was uncomplicated, and she was discharged after five days. She continues to do well.

Figure 1. Minimal scarring was encountered on initial inspection of the case patient’s chest at the time of completion pneumonectomy in 2015.
Increasing utilization of thoracic CT scans by a host of healthcare providers, together with the advent of Medicare reimbursement for screening CT scans in smokers, has led to the diagnosis of growing numbers of early lung cancers.
These cancers require a multidisciplinary treatment team that includes a thoracic surgeon. In many cases the patient and referring physician expect the surgeon to treat the cancer with a minimally invasive procedure, as such procedures have been shown to reduce postoperative pain and hasten recovery from surgery.

Figure 2. Completion pneumonectomy in the case patient was performed using video-assisted thoracoscopic surgery. This intraoperative photo shows a surgical stapler around the main artery entering the left lung.
Advertisement

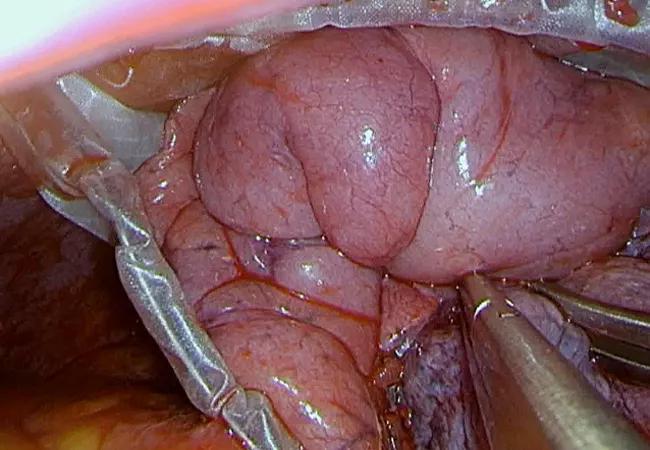
Figure 3. Intraoperative photo showing the remaining portion of the case patient’s lung being placed in a bag for extraction from the chest.
Indeed, the majority of patients with early-stage lung cancers can be treated with VATS or robotic surgery. In fact, virtually every oncologic disease of the lung and esophagus — as well as benign disease of the chest — can be treated with a minimally invasive approach. Likewise, minimally invasive techniques are widely used for mediastinal surgery and for biopsies of masses and lymph nodes. As a result, I perform 80 to 90 percent of my thoracic operations with video assistance.
At the same time, although the indications for minimally invasive thoracic procedures continue to expand, there remain clear indications for open surgery. My goal in choosing between the two is to achieve the necessary diagnostic and therapeutic outcomes for each patient while ensuring safety and a rapid recovery.
1) Improved functional outcomes. Compared with open surgery, less-invasive options such as VATS and robotic surgery result in reduced postoperative discomfort and quicker patient recovery. In turn, patients stay fewer days in the hospital and return to normal activities, including work, sooner.
2) Easy conversion to open surgery when needed. We expect minimally invasive thoracic surgery to become the gold standard for treating lung cancer. In addition to being easier on patients, minimally invasive techniques do not compromise the safety or quality of the cancer operation when applied appropriately. These procedures are easily converted to an open thoracotomy if the surgeon encounters any issue that might compromise the operation’s quality or safety.
Advertisement
3) Less-compromised anatomy if future procedures are needed. The case study above illustrates an overriding consideration in favor of minimally invasive thoracic surgery: leaving the patient better prepared for a possible future surgery. Because our patient’s initial cancer had been treated with VATS, she had minimal scar tissue in her chest (Figure 1). Although the appearance of an unrelated cancer four years later was unanticipated, lack of scar tissue meant the remaining portion of her lung could be successfully removed in a second minimally invasive procedure.
The optimal choice for an individual patient is dictated by his or her presenting anatomy, cancer stage, underlying physiologic status and history of prior chest surgeries and lung diseases.
Factors that may lead to preference for an open operation over a minimally invasive technique include:
Additionally, operations for mesothelioma and chest wall resections require open surgery at this time.
The surgeon’s experience and preference play a large role in patient selection, since the appropriate choice of any method depends on good surgical judgment. Individual surgeons and institutions must monitor their own outcomes, and such monitoring is enhanced by voluntary participation in the Society of Thoracic Surgeons (STS) General Thoracic Surgery Database. These outcomes data, together with the publicly reported STS quality ratings derived from them, can help patients make informed decisions.
Advertisement
The referring physician is wise to inquire whether a thoracic surgeon employs minimally invasive techniques, as the ability to offer a spectrum of options can help ensure the most appropriate oncologic care for a given patient.
Patients should be reassured that it is perfectly acceptable to ask a surgeon what percentage of procedures he or she performs minimally invasively — as well as the criteria used to decide when to use these techniques.
Consideration should also be given to whether the thoracic surgeon is part of a multidisciplinary team, since all oncologic surgeries benefit from a team approach. A team where the thoracic surgeon works closely with a medical oncologist, a radiation oncologist and a pulmonologist is best equipped to provide optimal care.
Dr. Raymond is a surgeon in the Department of Thoracic and Cardiovascular Surgery.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable