Pursuing a potentially treatable common pathway
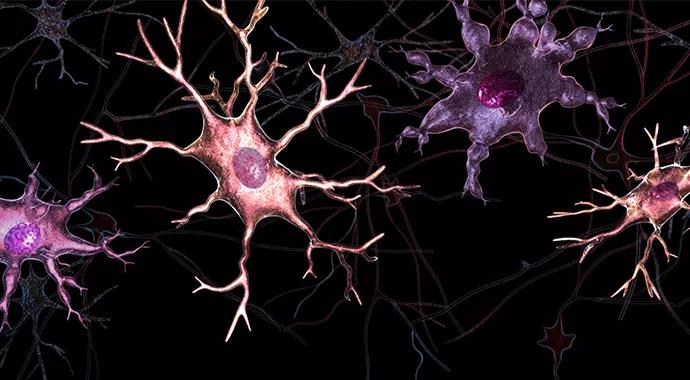
Promising research by Cleveland Clinic investigators demonstrates that microglial inflammation is a common pathway ‒ and a potentially treatable one ‒ for neuropathic pain and other treatment-resistant neuroinflammatory conditions, including Alzheimer disease (AD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Microglial inflammation is a mechanism of many CNS disorders ‒ neuropathic pain, AD, multiple sclerosis, parkinsonism, you name it,” says lead researcher Mohamed Naguib, MD, of Cleveland Clinic’s Anesthesiology Institute, which includes the Department of Pain Management.
His team has synthesized a molecule called MDA7, a cannabinoid type 2 (CB2) receptor-selective agonist, to inhibit microglial inflammation in hopes of effectively treating neuropathic pain and other conditions. “MDA7 prevents microglial activation and recruitment, which represent the elemental pathway of microglial inflammation,” explains Dr. Naguib.
The researchers demonstrated as much in a 2012 paper in Anesthesia and Analgesia (2012;114[5]:1104-1120) reporting findings from a rodent model of paclitaxel-induced neuropathy, which is associated with activation of microglia followed by the activation and proliferation of astrocytes and the expression and release of pro-inflammatory cytokines. They found that MDA7 prevented paclitaxel-induced allodynia in rats and mice in a dose- and time-sensitive fashion without compromising paclitaxel’s anticancer effects. MDA7’s anti-allodynia effect was absent in CB2–/– mice and was countered by CB2 antagonists, which suggests it directly involves CB2 receptor activation.
Because all neuropathic pain shares the mechanism of microglial inflammation, Dr. Naguib expects the same effect in neuropathic pain types outside the chemotherapy setting. “We started with chemotherapy-induced neuropathy because it’s an area of unmet therapeutic need,” he says.
Advertisement
His team recently finished a study using a vascular occlusion model in the rat to replicate another form of chronic pain with a microglial inflammation mechanism, complex regional pain syndrome (CRPS). MDA7 was again highly effective, both at the molecular level and in terms of phenotypic response. They expect to submit the CRPS study for publication this year.
The wider biomedical community learned of the team’s work via an exciting study in February’sNature Neuroscience (2014;17[2]:223-231) linking microglia-mediated inflammatory changes in a postsynaptic protein, neuroligin 1, to amyloid-associated memory deficiency in rodents.
Current models of AD hold that amyloid plaques accumulate in the brain, overwhelming the microglia that serve as the nervous system’s main form of active immune defense. When the microglia cannot clear out amyloid rapidly enough, they become inflamed, which leads to gene modifications in the brain.
“As our research into microglial inflammation advanced, it became clear how important this inflammation is to a variety of disease processes, which led down the Alzheimer path,” says Dr. Naguib.
His team’s Nature Neuroscience study showed that the microglial inflammation-induced gene changes in the brain include suppressed expression of the neuroligin 1 protein ‒ and that this suppression leads to hippocampal glutamatergic dysfunction and memory deficiency in rodents. The effects were ameliorated by inhibiting microglial activation. “These findings link neuroinflammation, synaptic efficacy and memory, thus providing insight into the pathogenesis of amyloid-associated diseases,” the researchers concluded.
Advertisement
Dr. Naguib notes that much research remains, but the findings suggest that MDA7 represents a promising new therapeutic approach to AD and other conditions involving microglia-mediated neuroinflammation, such as multiple sclerosis and Parkinson disease.
In the near term, the researchers are focused on gaining funding to move MDA7 into phase 1 human studies for chemotherapy-induced neuropathy, which they hope to begin by 2015. Studies of MDA7 in animal models of AD will take longer, due to the longitudinal nature of AD, but Dr. Naguib says the team is committed to pursuing that research as well.
Mohamed Naguib, MD is a professor of anesthesiology in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade