MIS technique provides an alternative to watchful waiting or lobectomy
The use of CT to screen for lung cancer has enabled detection of lesions at increasingly smaller sizes. Yet that positive development brought along with it a clinical conundrum: “Until recently, patients with very small lesions were told that their only option was to wait until the lesion could be palpated before having it removed,” says Cleveland Clinic thoracic surgeon Daniel Raymond, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That was before the advent of an innovative procedure that’s rapidly changing the diagnostic and treatment picture for patients with very small nodules and ground-glass lung lesions. The procedure, known as microcoil localization or by several alternate names (nodule localization, needle localization, fiducial localization), allows thoracic surgeons to accurately resect these lesions in a minimally invasive fashion.
“We’re no longer dependent on lesions being palpable to pinpoint their location,” notes Dr. Raymond. “Wire localization enables us to localize questionable areas, remove them thoracoscopically and make a diagnosis.”
Percutaneous nodule localization is a complex technique offered at Cleveland Clinic and a small number of other U.S. centers. It requires close teamwork between a radiologist, who locates the nodule and places the microcoil, and a thoracic surgeon, who removes the lesion.
The primary team at Cleveland Clinic — consisting of Dr. Raymond, thoracic surgeon Sudish Murthy, MD, PhD, and thoracic radiologist Jason Lempel, MD — has performed the procedure on approximately 60 patients since February 2015. All Cleveland Clinic thoracic surgeons and one additional thoracic radiologist have since been trained on details of the procedure.
“Microcoil localization isn’t the first attempt at developing a technique to enable pinpointing of small lesions, but we have found it to be the best and most accurate option,” says Dr. Lempel.
Percutaneous microcoil localization and subsequent video-assisted thoracoscopic surgery (VATS) resection is performed in two stages:
Advertisement

Figure 1. CT localization image showing a ground-glass nodule with a localizing microcoil (arrow) extending from the nodule back to the pleural surface and marking the nodule for subsequent VATS resection.
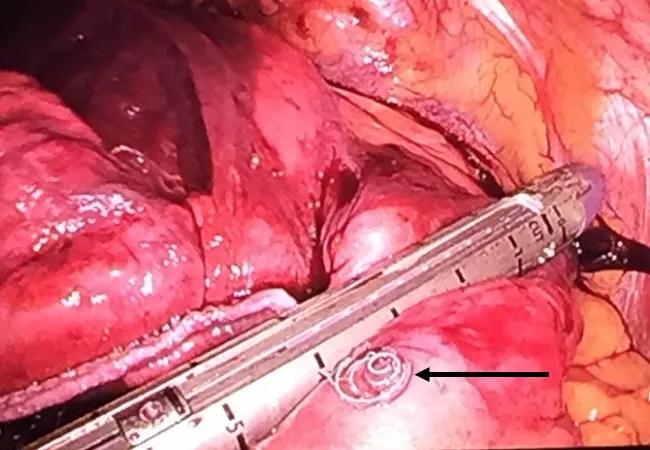
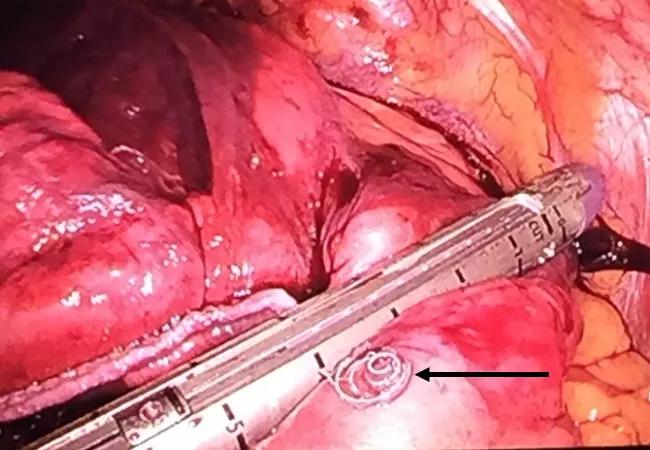
Figure 2. Intraoperative photograph showing a coil along the pleural surface (arrow) guiding the surgeon to the precise location for wedge resection.
At Cleveland Clinic, the resection is usually done without fluoroscopic assistance, as the radiologist tells the surgeon how many centimeters from the surface of the lung the distal end of the microcoil is located.
“We could use fluoroscopy to confirm that the cut is around the deep end of the coil, but it’s preferable to limit radiation exposure to the patient and surgical staff whenever possible,” Dr. Lempel explains.
In fact, a review of the team’s first 20 cases confirmed a 100 percent success rate in retrieving the target lesion with clear margins.
The optimal environment for this complex procedure is still being worked out. Drs. Raymond and Lempel have tried two protocols.
In one, the patient is placed under conscious sedation and the localizing coil is inserted in the radiology suite. The patient is then transferred to the OR and anesthetized for the resection.
The alternate method — and their preference — is to perform both stages of the procedure in one of Cleveland Clinic’s hybrid ORs. This allows the patient to be anesthetized for the entire procedure, with the anesthesiologist controlling ventilation to obtain minimal motion of the lung during the procedure.
Advertisement
No matter where needle localization is performed, its advantages are clear:
As the team continues to accrue experience with microcoil localizations, Dr. Raymond is cautiously optimistic about its long-term outcomes. “The classic treatment is lobectomy,” he says. “However, the probability of lymph node disease with these very small lesions is low, so a wedge resection may be all that’s necessary.”
“I believe microcoil localization will eventually eliminate the need for lobectomy and conversion to open thoracotomy in many of these situations,” adds Dr. Lempel. “We’re achieving clean margins with the minimal amount of tissue resected.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable