Measuring residual risk of adverse perivascular adipose tissue remodeling
A novel biomarker derived via machine learning can predict cardiac risk better than currently available risk prediction methods, according to a study presented at the 2019 European Society of Cardiology Congress in Paris and simultaneously published online by the European Heart Journal. Using artificial intelligence, researchers analyzed both tissue and imaging features to identify markers of perivascular fat remodeling, connect those markers to cardiac risk and then develop a single value to express that risk.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, conducted by researchers at the University of Oxford working with colleagues in Germany and at Cleveland Clinic, builds on the groundbreaking work of the Cardiovascular Risk Prediction using Computed Tomography (CRISP-CT) study, which established a perivascular fat attenuation index (FAI) that can predict all-cause and cardiac mortality above and beyond clinical risk factors and current coronary CT angiography (CCTA) interpretation methods.
The current study adds perivascular fat fibrotic and microvascular changes to the inflammation quantified by FAI to achieve a fat radiomic profile (FRP). This “radiome,” a machine learning-derived combination of biological, tissue-derived features and imaging features, can predict future coronary events with great accuracy.
“This is a significant advance in the field,” says co-author Milind Desai, MD, Professor of Medicine at Cleveland Clinic Lerner College of Medicine and a Cleveland Clinic cardiologist. “The new marker extracts additional information about underlying pathology from routinely obtained scans. This type of artificial intelligence-based technology could represent a big step forward in personalized care for people predisposed to future coronary events.”
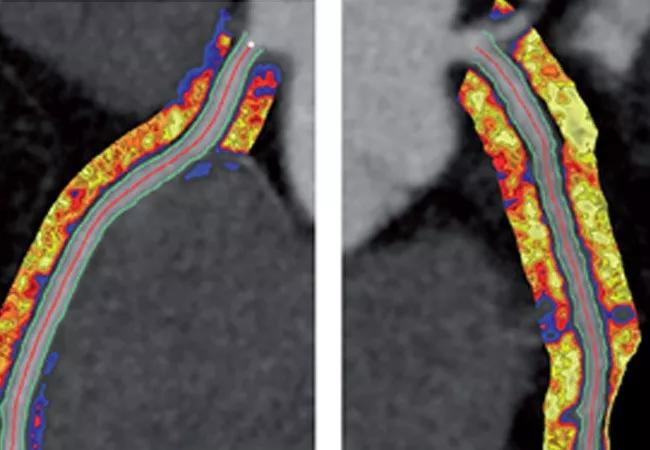
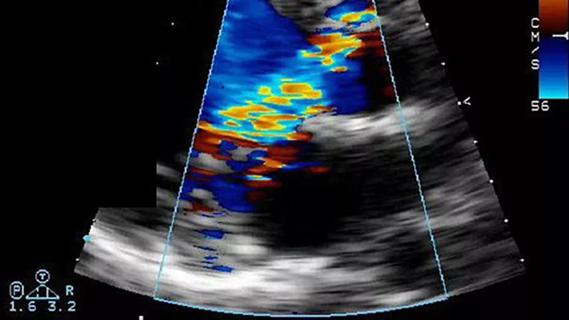
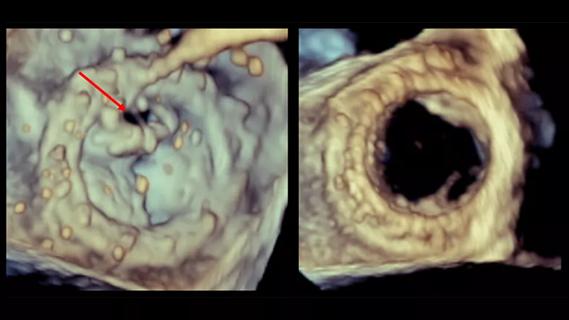
In the first of three phases of the study, investigators performed genetic transcription studies on fat biopsies from 167 patients undergoing cardiac surgery. They also analyzed radiographic features from the patients’ CCTA images (see examples at top of post). The resulting analysis linked the CCTA radiomic features to genetic markers of perivascular fat fibrosis, inflammation and vascularity.
Advertisement
The second phase of the study applied this analysis to patients from the CRISP-CT and Scottish Computed Tomography of the HEART (SCOT-HEART) trials to develop and validate a marker —the FRP — that could encapsulate relevant tissue and imaging factors in a single value. The researchers designed a case-control study that matched 101 patients who had a major cardiac adverse event (MACE) within five years of CCTA to 101 similar patients who did not have a cardiac event during the same period. Patients were split into training and internal validation (80%) and external validation (20%) sets. The investigators then used a random forest machine learning model to build the FRP.
Once the FRP was established, the researchers tested its mettle among 1,575 patients from SCOT-HEART. They found that over median follow-up of almost five years, an FRP above a certain tested threshold was associated with an almost 11-fold increase in MACE risk. This association held even after controlling for a variety of traditional cardiac risk factors, including diabetes mellitus, smoking, body mass index, obstructive disease and total cholesterol, among others.
With the FRP developed and verified, the third phase of the study evaluated whether this marker could also detect unstable coronary plaques and track longitudinal changes in perivascular fat structure. Radiomic phenotyping was performed on 44 patients who underwent CCTA within 96 hours of admission for acute myocardial infarction (AMI), as well as on 44 matched controls with CCTA results from workup for stable coronary artery disease. Patients in the AMI group had higher FRP values. Longitudinally, there were no significant changes in the FRP value for 16 patients who had CCTAs both from 96 hours post-AMI admission and at a six-month follow-up visit.
Advertisement
“Looking at the follow-up scans of these patients at six months, we found that their fat radiomic profiles remained the same while their fat attenuation index decreased significantly,” notes Dr. Desai. “We think the FRP captures permanent changes in perivascular fat composition, which, when paired with the fat attenuation index, gives us a more comprehensive cardiac risk profile for each patient.”
The development of a machine learning-powered way to measure cardiac risk through analysis of perivascular fat is novel, and the validation of the resulting method — the FRP — in patient cohorts from multiple studies makes a compelling case for its exploration in clinical practice.
“Machine learning techniques unlock a wealth of data in cardiac imaging and tissue analysis,” observes Brian Griffin, MD, Section Head of Cardiovascular Imaging at Cleveland Clinic and another co-author of the study. “That FRP allows us to predict adverse clinical events more accurately than anything else currently available is a major advance in how we understand perivascular structural remodeling. More importantly, it’s a major step forward in patient care in both primary and secondary prevention.”
Images of coronary artery perivascular adiopose tissue at top are reprinted from Oikonomou et al., European Heart Journal (doi:10.1093/eurheartjehz592), © The authors, 2019.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
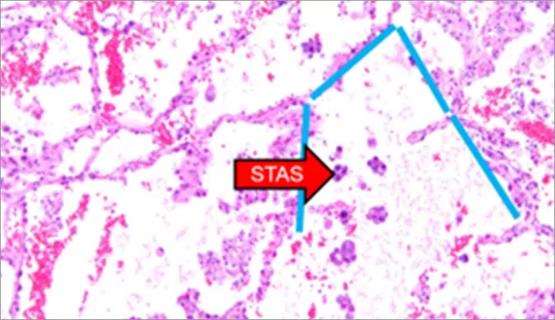
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable