Experienced team, comprehensive evaluation are critical
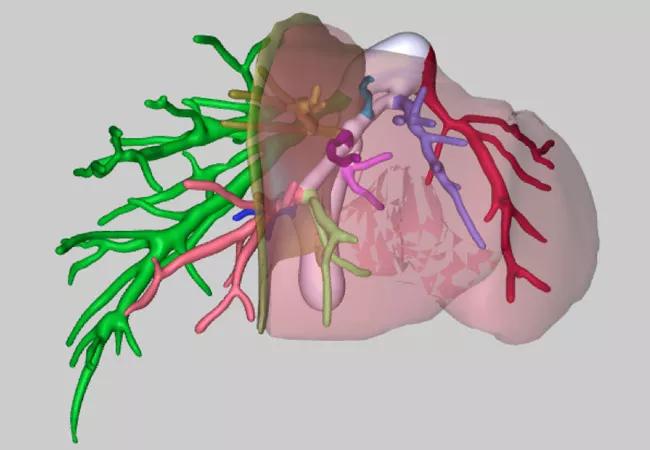
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/60fe281d-2b3c-4917-9c25-6661aca99112/17-DDI-3738-Hashimoto-CQD-1_jpg)
17-DDI-3738-Hashimoto-CQD-1
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Living donor liver transplantation (LDLT) helps patients who don’t have priority on the transplant waiting list receive life-saving liver transplantation in a timely fashion.
Because a small, partial graft may cause small-for-size graft failure, the larger right lobe (65 to 70 percent of a whole liver) has been generally used in adult-to-adult LDLT worldwide. However, right lobe living donation has significant risks of morbidity and mortality in living donors.
Although the use of left lobe grafts (30 to 35 percent of a whole liver) is safer for living donors because the amount of liver volume taken from donors is smaller, the risk of graft failure is higher when a left lobe is used for adult recipients.
At Cleveland Clinic, we have achieved excellent outcomes in left lobe LDLT, and have particular experience in this field.
The patient is a 69-year-old male who had end-stage liver disease secondary to cryptogenic cirrhosis.
He had severe portal hypertension but did not have priority on the liver transplant waiting list. His friend became a living donor for him.
After comprehensive donor and recipient evaluation including 3-D simulation of liver anatomy, he received a left lobe graft with a graft-to-recipient weight ratio (GRWR) of 0.53 percent. Since the lowest limit of GRWR for LDLT is generally considered to be between 0.7 percent and 0.8 percent, there is no transplant center that routinely uses living donor grafts with a GRWR < 0.6 percent.
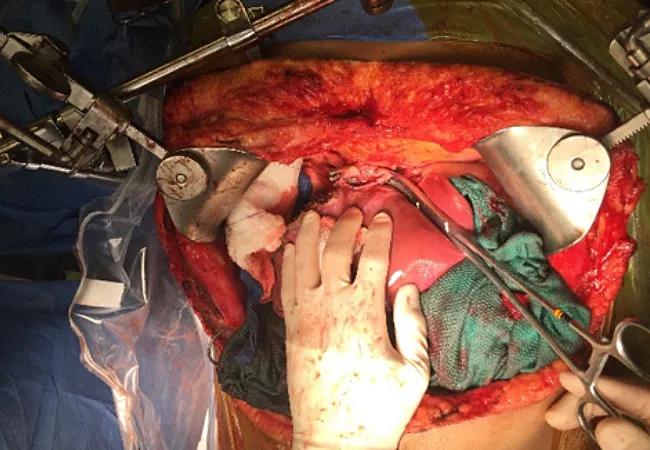
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ace59eaa-3e04-4198-99a3-8771d13b7bb4/17-DDI-3738-Hashimoto-CQD-2_jpg)
The patient did very well after transplant, without signs of small-for-size graft failure. A postoperative CT scan showed the left lobe graft has regenerated and now is as big as his native whole liver.
Advertisement
Advertisement
Advertisement
Strong patient communication can help clinicians choose the best treatment option
ctDNA should be incorporated into care to help stratify risk pre-operatively and for post-operative surveillance
The importance of raising awareness and taking steps to mitigate these occurrences
New research indicates feasibility and helps identify which patients could benefit
Treating a patient after a complicated hernia repair led to surgical complications and chronic pain
Standardized and collaborative care improves liver transplantations
Fewer incisions and more control for surgeons
Caregiver collaboration and patient education remain critical