Study reveals a way to predict recovery in the long term
Late recovery of atrioventricular (AV) conduction after cardiac surgery and subsequent pacemaker placement is not uncommon and is not related to surgery type. So concludes the largest study to date investigating late AV conduction recovery and the first to examine its clinical predictors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, presented at the American Heart Association’s Scientific Sessions 2016 in New Orleans by Cleveland Clinic electrophysiologist Daniel J. Cantillon, MD, also suggests that a simple presurgical ECG measurement might be useful for predicting whether a patient will recover conduction in the long term if a pacemaker is required.
About 5 percent of patients undergoing heart valve surgery and 1 percent of those undergoing coronary artery bypass grafting develop postsurgical complete heart block requiring pacemaker implantation. Late recovery of AV conduction — i.e., between one and six months postsurgery — in such patients is considered exceptional, “but patterns of late recovery have been poorly defined,” explains Dr. Cantillon.
To get a better handle on those patterns, Dr. Cantillon and colleagues reviewed consecutive patients who received a pacemaker for complete heart block following cardiac surgery at Cleveland Clinic from 2000 to 2014. Patients had to receive the pacemaker during their index hospitalization, and individuals with biventricular pacemakers were excluded.
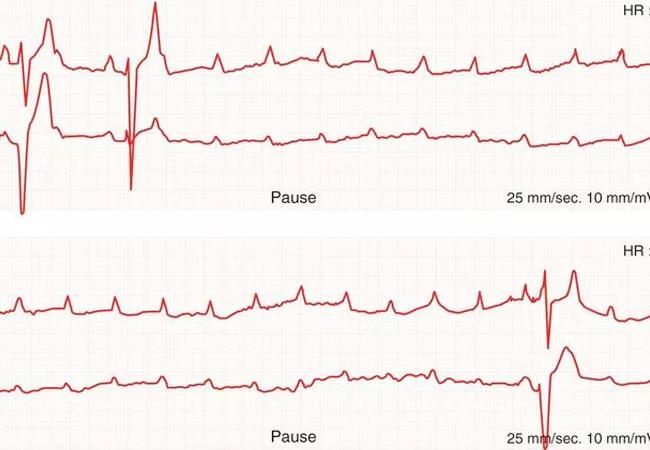
The primary end point was AV nodal conduction recovery, defined as a reduction in ventricular pacing to less than 10 percent at least one month after pacemaker implantation. Multivariable logistic regression analysis was performed to identify predictors of late recovery among variables ranging from patient demographics and medical history to surgical subtype and pre-/postsurgical ECG findings.
The study’s inclusion criteria were met by 326 patients (mean age, 66 ± 14 years; 57 percent male), with mean follow-up of 4.2 years. Analysis of outcomes among these patients yielded the following insights:
Advertisement
“Findings in this study were surprising in several ways,” says Dr. Cantillon. “We expected to find differences in late AV conduction recovery based on type of surgery. Instead we found that only two clinical factors were associated with late recovery: female gender and whether or not the patient had evidence of transient AV conduction after surgery.”
Apart from an association with tricuspid valve surgery, the researchers found no broad differences in late recovery rates related to type of surgery — whether bypass, valve, myectomy, TAVR or reoperation — or surgical approach (transcatheter versus open).
The researchers also identified a simple electrical parameter that can be measured before surgery to potentially guide clinical decision-making. “If a patient has both a PR interval longer than 200 msec and a QRS duration greater than 120 msec on ECG, there is no chance he or she will recover conduction in the long term,” Dr. Cantillon says.
He adds that this simple measure “can help clinicians understand whether this is a patient in whom you can implant a transvenous pacemaker and feel very comfortable that it will be needed for rest of the patient’s life, regardless of gender, type of surgery, etc. We believe this is a robust, confidence-building finding that can assure us whether we are doing the right thing.”
Dr. Cantillon notes that, currently, pacemaker recipients who experience late AV conduction recovery will retain the device in situ for the rest of their lives. Although patients with pacemakers generally have a very good quality of life, approximately one in 10 will experience a problem with lead wires or the surgical pocket over the long term. “While the pacemaker is essential at the time of implantation,” he says, “those who no longer need pacing down the road still face a potential hazard without a counterbalancing benefit.”
Advertisement
Ultimately, Dr. Cantillon and other researchers hope to identify patients who may not need a permanent pacemaker or might be candidates for leadless pacemakers that can be removed once AV block resolves. “This study was a first step toward developing this type of bridge pacing strategy for patients likely to recover,” he says.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable