Meta-analysis proves its value, but patient risk defines its role
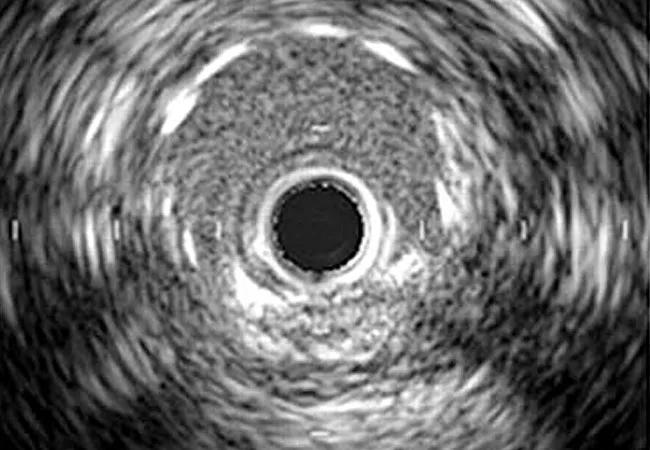
Does the superiority of intravascular ultrasound (IVUS) over angiography for guiding percutaneous coronary intervention (PCI) apply in the era of drug-eluting stents?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

Stephen Ellis, MD
Until recently, there was no definitive answer. But a carefully conducted meta-analysis to address that question, published by University of Florida researchers in the April 2016 Circulation: Cardiovascular Interventions, has signaled that the answer is yes.
Consult QD asked veteran Cleveland Clinic interventional cardiologist Stephen Ellis, MD, to provide some context for the analysis and weigh in on what its implications for clinical practice may be.
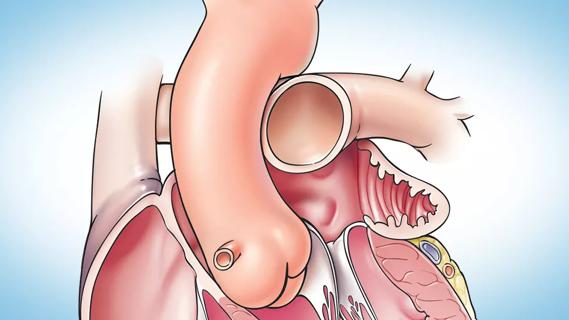
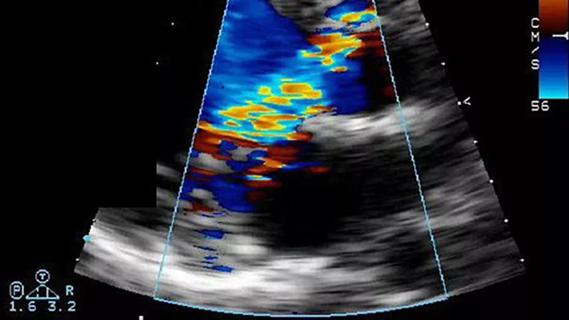
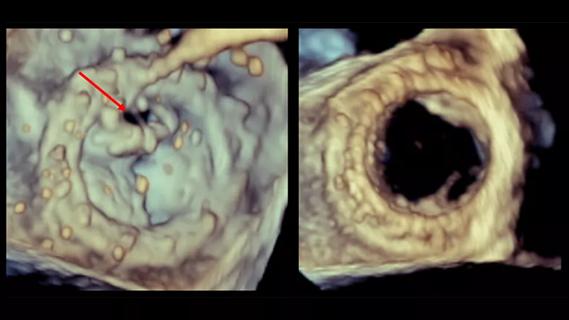
Dr. Ellis: Angiography is the traditional modality for visualizing the severity of coronary lesions before, during and after PCI. Yet operators are aware that angiography doesn’t allow for sufficient visual assessment of a coronary lesion. IVUS is a more sensitive tool that allows for optimization of stent implantation by ensuring good stent expansion and apposition.
A few years ago, a meta-analysis of randomized controlled trials (RCTs) involving bare-metal stents found that IVUS-guided PCI reduced major adverse cardiac events and revascularizations compared with angiography-guided PCI.
PCI is now performed with drug-eluting stents, which significantly lower restenosis risk relative to bare-metal stents, raising the question of whether the incremental benefit of IVUS-guided PCI over an angiography-guided approach still applies in the era of drug-eluting stents. Previous meta-analyses that included drug-eluting stents failed to show benefit, but these analyses included a limited number of trials and were tainted by the inclusion of observational studies.
Advertisement
Dr. Ellis: The new meta-analysis in Circulation: Cardiovascular Interventions excluded observational studies and included all RCTs of drug-eluting stents published to date — seven in all, with a total of 3,192 patients. They involved a mix of first- and second-generation drug-eluting stents.
The analysis showed that IVUS-guided PCI was associated with a reduced risk of adverse cardiac events compared with angiography-guided intervention. Benefit was driven primarily by a significant reduction in target-lesion revascularization (4.1 vs. 6.6 percent; odds ratio = 0.60 [95% CI, 0.43-0.84]), although IVUS guidance was also associated with lower risks of cardiovascular mortality (0.5 vs. 1.2 percent) and stent thrombosis (0.6 vs. 1.3 percent). IVUS guidance also resulted in more frequent postdilatation, producing a greater minimum lumen diameter.
Dr. Ellis: I was not surprised to see benefit, although I was surprised at the magnitude of the benefit.
Dr. Ellis: It does. You can see how well the stent is expanded, and the minimum lumen area in the stented segment is strongly correlated with the need for revascularization. You may think you have a good result, but you may need to go back in.
Dr. Ellis: No. At Cleveland Clinic, we generally use it only on high-risk lesions, in patients at highest risk for restenosis. In those cases, it’s a good idea.
Dr. Ellis: The American College of Cardiology/American Heart Association recommendation for use of IVUS in left main coronary artery stenting and for assessment of nonleft main intermediate coronary stenosis is currently a class IIb recommendation, and it will probably remain that way. The RCTs in this meta-analysis did not include typical patients: They were highly selected, high-risk patients. The risk with run-of-the-mill patients may be overestimated.
Advertisement
Dr. Ellis: The meta-analysis paper cites 2012 National Cardiovascular Data Registry numbers showing that IVUS was used in about 20 percent of all PCI procedures at that time. In 2015, the rate of usage nationwide was 13 percent.
As the paper points out, cost and the additional time required are likely relevant factors limiting broader use. Also, interpretation may not be straightforward for lower-volume operators, and that may be a factor. Additionally, some hospitals may not have IVUS capabilities.
Dr. Ellis: Relatively new edge-enhancement software programs with angiography — known as “stent boost systems” — allow much better angiographic assessment of stent expansion than before. This “poor man’s IVUS” may well minimize the incremental benefit of IVUS, although that remains to be better studied.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
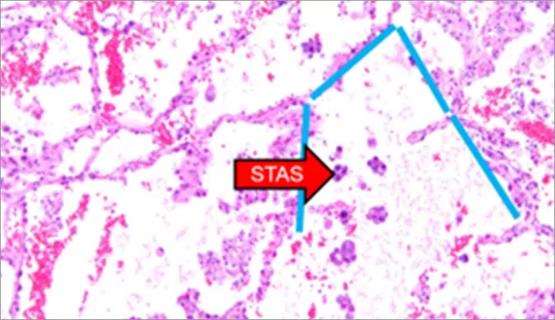
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable