A minimally invasive, single-incision approach to two coexisting problems
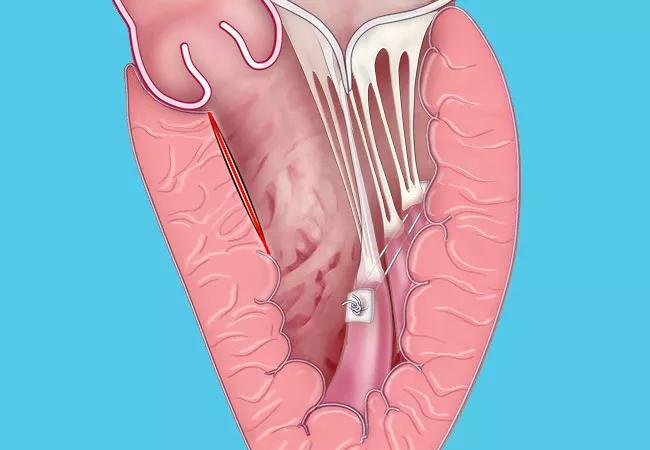
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/21d2f178-9154-429a-a145-244248715b9b/20-HVI-1941484_robotic-myectomy-mitral-valve-repair_650x450_jpg)
20-HVI-1941484_robotic-myectomy-mitral-valve-repair_650x450
Patients with hypertrophic obstructive cardiomyopathy (HOCM) who require myectomy along with mitral valve (MV) repair are being treated at Cleveland Clinic with a new minimally invasive, robotically assisted procedure performed through a single incision.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Typical candidates need a septal myectomy but also have a prolonged anterior mitral leaflet and an abnormal, hypermobile papillary muscle in addition to the need for mitral valve repair,” explains Cleveland Clinic cardiothoracic surgeon Per Wierup, MD, PhD, who led efforts to develop the procedure. “If they have this combination of features, and no contraindications for robotic surgery, they are ideal patients for this approach.”
He finds the opportunity to correct two problems through a single incision in a minimally invasive operation highly appealing. “It is a safe alternative to a well-established open heart procedure that allows patients to retain their own valve and leaves them with a septum of normal thickness,” he says. “Because the aortic valve is not touched, the potential complications from a trans-aortic septal myectomy are avoided.”
Dr. Wierup is one of the Cleveland Clinic cardiothoracic surgeons pushing the boundaries of robotically assisted heart surgery. To date, they have performed more than 2,000 robotic MV repairs. This unparalleled experience has enabled them to master the procedure. “Patients who come to us needing mitral valve surgery typically receive a robotic repair,” he says.
Cleveland Clinic surgeons also have performed thousands of myectomies, primarily as open heart procedures using a trans-aortic approach. It was this deep experience in both robotic MV repair and trans-aortic myectomy that led Dr. Wierup and colleagues to consider correcting both defects through a single incision in a robotically assisted procedure.
Advertisement
Following the lead of robot-assisted myectomy pioneer Randolph Chitwood, MD, Dr. Wierup performed the first combined myectomy and MV repair with robotic assistance in September 2019. He has since done two additional procedures, all with excellent outcomes.
“The patients spent one day in the ICU and were discharged after three or four days,” Dr. Wierup notes.
Left ventricular outflow tract obstruction (LVOTO) in HOCM can be aggravated by systolic anterior motion of the anterior MV leaflet. “The anterior leaflet is sucked toward the septum, further obstructing outflow,” says Dr. Wierup.
Combining septal myectomy with reorientation of the papillary muscles can decrease LVOTO. However, the surgery typically requires a full sternotomy for the myectomy. The heart must then be opened in a second location to repair the MV.
The new robotically assisted approach was designed to simplify this operation. Dr. Wierup and colleagues detail the surgical approach in a recent article in the Journal of Cardiac Surgery, which includes the illustrations in the figure below. “We can see the valve and septum exceedingly well,” he says. “The visualization is fantastic.”
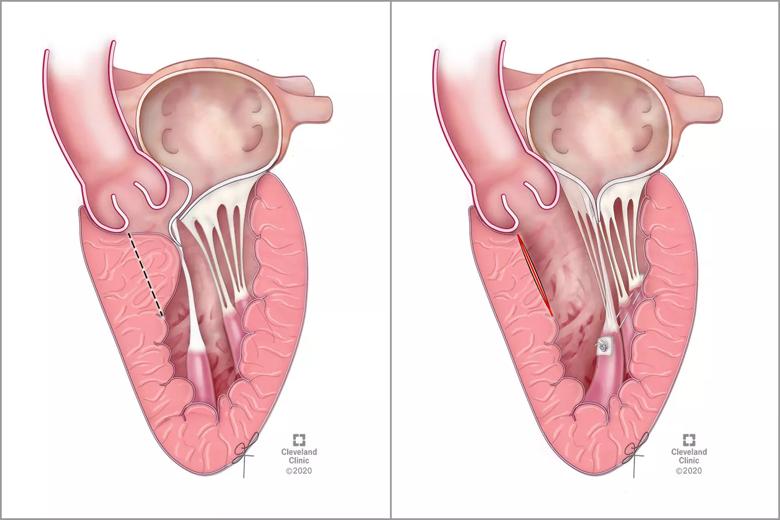
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/17ae2b46-1cc6-44f9-abbe-0c51cd59f7ea/20-HVI-1941484_robotic-myectomy-plus-mitral-valve-repair_inset_jpg)
Figure. Illustrations before (left) and after (right) robotic myectomy with mitral valve repair. The left panel shows HOCM and systolic anterior motion from anterior papillary muscle, with the dashed line indicating the planned resection line. The right panel shows postoperative reorientation of the papillary muscle heads. Reprinted from Kumar et al., J Cardiac Surg. (Epub 2 Aug 2020). © 2020 Cleveland Clinic Foundation.
Advertisement
At Cleveland Clinic, HOCM patients with severe septal hypertrophy continue to undergo septal myectomy performed through a median sternotomy. When the primary problem is MV disease and the patient also has HOCM, they are treated with the minimally invasive robotic approach.
“This gives us two options,” Dr. Wierup says. “Many other institutions that do surgery for HOCM believe only the muscle should be cut out. From this standpoint, we are alone in taking a holistic approach.”
That may change, however, as demand for minimally invasive procedures continues to grow. Yet Dr. Wierup cautions that familiarity with robotic technique is not sufficient for success in robotic myectomy with MV repair; a huge experience in myectomies is also needed.
“These are tricky problems, because fixing one problem can make the other worse,” he explains. “You have to find a good balance, which takes experience-based judgment in addition to the foundational technical ability.”
“This is a much-needed development in the management of obstructive hypertrophic cardiomyopathy, especially since many such patients tend to be younger and would like to return to work sooner and have a less-visible chest scar,” notes Milind Desai, MD, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center. “With the emergence of novel noninvasive therapies, we are entering an exciting phase of management of these patients.”
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable