Data show symptoms are markedly reduced within five weeks

By Kelly Davidson, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sometimes one psychotherapy session per week isn’t enough for adolescents dealing with mood disorders, even when they’re able to maintain daily functioning. They need a middle ground, something between inpatient treatment (for acute stabilization) and standard outpatient visits. For these teens, Cleveland Clinic’s Center for Behavioral Health offers its Adolescent Mood Disorders Intensive Outpatient Program (adolescent IOP).
Our adolescent IOP is similar to adult IOPs, with one important addition: sessions for parents. While adult patients aren’t always receptive to family involvement, parental or guardian involvement is crucial for teen patients.
Patients ages 13 to 17 (or 18 if still in high school) who are diagnosed with a mood disorder can be part of the adolescent IOP hosted at Cleveland Clinic Lutheran Hospital on Cleveland’s West Side. Sessions are three hours each, held after school Mondays through Thursdays.
The teens meet in a group where they learn and practice cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) skills to help navigate issues at school or home. As needed, therapists can provide individual coaching to help patients better engage in the group, or family meetings to help families navigate more complex psychosocial issues.
Enrollment is always open, with referrals coming from both inpatient units and outpatient providers. There is no waiting list. Average attendance is eight to 10 teens per session.
Unlike other IOPs, our program directs each patient’s complete psychiatric care during treatment. A psychiatrist or nurse practitioner provides regular medication management.
Advertisement
The average length of stay in the adolescent IOP is 20 sessions — about five weeks. That allows our staff ongoing observation of patients’ symptoms, family dynamics and response to interventions. Patients then return to regular outpatient care.
Often we find that parents are uninformed or misinformed about diagnosis, treatment and how to best support their teen with a mood disorder. But parental involvement is an important part of treating these kids.
I tell them that they and their kids are a team, and kids are reliant on parents to do their part, especially when they live in the same household. If the teen is able to change but the parent doesn’t also grow and adapt, the teen’s symptoms may resume.
That’s why our adolescent IOP includes a weekly one-hour session to educate parents on:
Our program also partners with the National Alliance on Mental Illness (NAMI) to provide peer support for parents.
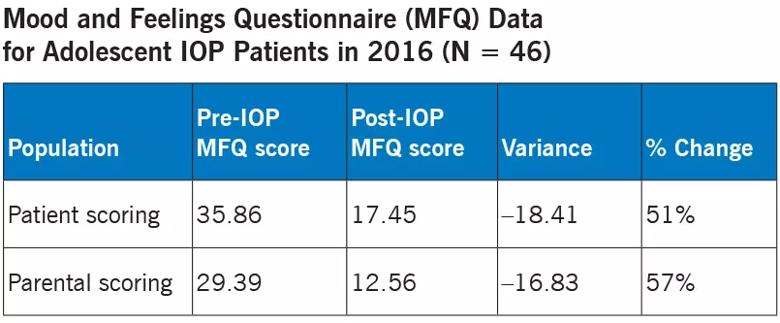
In 2016, we began administering the Mood and Feelings Questionnaire (MFQ) to patients and their parents at the beginning and end of the adolescent IOP. On average, patients’ MFQ scores improved (symptoms decreased) by 49 percent from start to end of treatment. Parents’ perceptions of their child’s mood symptoms improved by 43 percent. Specific score data are outlined below.
Advertisement
Now we are administering the MFQ to patients each week so we can chart changes during the course of IOP treatment. We share data with parents to show our progress. Parents have remarked that these data are valuable since progress in psychiatric treatment often can seem subjective.
From 2016 to 2017, our average daily census has increased 45 percent. In some months referrals are up more than 100 percent. I attribute that achievement primarily to changes we’ve made in response to patient and parent feedback, including:
We continue to solicit feedback and track patient satisfaction scores, which in 2016 exceeded national averages from the Association for Ambulatory Behavioral Healthcare across all domains assessed.
Patient engagement and satisfaction are intimately related to identifying and meeting the needs and wants of patients and their families.
To refer a patient to the adolescent IOP, call 216.828.5400. A therapist will contact the patient’s legal guardian within one business day to schedule an intake assessment.
Dr. Davidson (shown in photo at top) is a child and adolescent psychiatrist who directs the adolescent IOP within Cleveland Clinic’s Center for Behavioral Health.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade