Analysis helps risk-stratify patients and prioritize if monitored bed resources are limited

Hospitalized patients who are at the highest risk for needing emergency response team care can be identified by their indication for cardiac telemetry monitoring, allowing prioritization of monitoring resources.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concludes an analysis of Cleveland Clinic’s experience with its system for cardiac telemetry monitoring of non-critically ill patients over a 13-month period, recently published online in Clinical Cardiology.
“Indication-specific event rates for cardiac-, noncardiac- and arrhythmia-related clinical deterioration among hospitalized patients are seldom reported, but identifying these rates allows patient risk stratification,” says the study’s lead author, Daniel Cantillon, MD, Medical Director of Cleveland Clinic’s Central Monitoring Unit. “This is especially important for hospitals with constrained resources, such as too few telemetry beds, or those that need to transfer high-risk patients to a facility with a higher level of care.”
A 2017 update to American Heart Association guidelines for electrocardiographic monitoring in hospitals (Circulation. 2017;136:e273-e344) included a call for more research. In response, Cleveland Clinic investigators analyzed data from their central monitoring unit, which provides remote cardiac telemetry monitoring of patients hospitalized in non-intensive care units at 11 hospitals in the Cleveland Clinic health system (as detailed in this previous Consult QD post).
The central unit was developed to address “alarm fatigue,” reducing the chance that an important alarm will be missed. With the assistance of risk-stratification tools and algorithms, dedicated technicians are trained to recognize important physiological changes. When appropriate, they alert nursing staff and, in more urgent situations, an emergency response team (ERT) consisting of a physician, a nurse and a respiratory therapist to quickly manage the patient or facilitate ICU transfer.
Advertisement
The new study analyzed 23 standardized indications for cardiac telemetry monitoring (listed in the article) at Cleveland Clinic’s main campus and two regional hospitals from March 2014 to April 2015, including various arrhythmias, high-risk coronary disease, heart failure and seizure monitoring, among others. ERT activations were systematically collected as an endpoint for clinical deterioration and categorized into cardiac and noncardiac groups, with further substratification into arrhythmia-specific events.
The data consisted of 72,199 telemetry monitoring orders and 2,677 ERT activations (3.7% of telemetry orders), 49.5% of which were for cardiac-related events.
Findings from the data analysis included the following:
Advertisement
The investigators also presented their findings as a bubble plot depicting telemetry order volume (indicated by bubble size) and overall ERT activation and cardiac-specific ERT activation rates (Figure). The plot’s right upper quadrant, indicating high overall and cardiac-related event rates, identifies indications with the greatest need for continuous cardiac monitoring, whereas the left lower quadrant identifies those with lesser need for continuous monitoring.
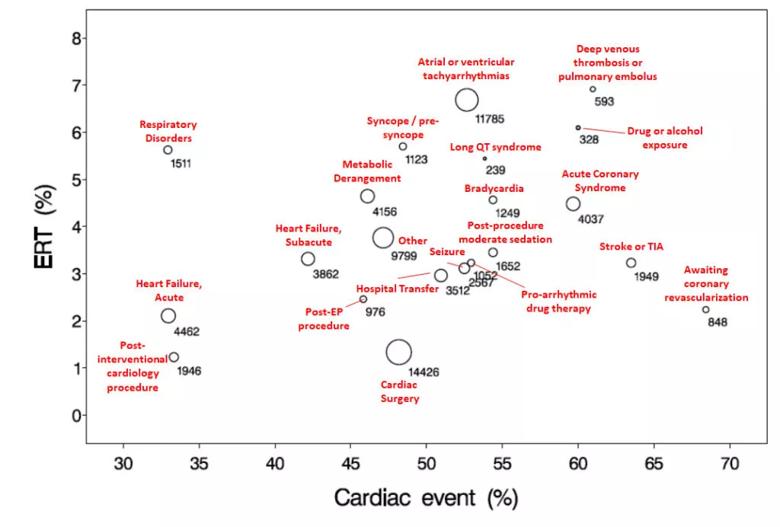
Figure. Bubble plot showing volumes for cardiac telemetry indications with rates of overall emergency response team (ERT) activations on the y-axis and cardiac-related ERT activations on the x-axis. See text for further explanation. Reprinted from Cantillon et al., Clinical Cardiology. doi:10.1002/cic.23244. ©2019 The authors.
According to the authors, this analysis provides evidence to update current guidelines for inpatient cardiac telemetry monitoring by:
“An important takeaway is that our analysis provides a method for prioritizing telemetry monitoring resources by patient indication that other institutions can adapt based on their patient populations and resources,” notes Dr. Cantillon.
Advertisement
“Inpatients’ indication-specific risk for clinical deterioration has been underexplored for too long,” adds Oussama Wazni, MD, Section Head of Electrophysiology and Pacing at Cleveland Clinic. “We hope this work starts to change that.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable